What should I be doing? I want my daughter to get the most out of school.
It’s a new year and I’m feeling positive. but then is that just me being me?
How we embrace the start of something new is dependent on so many factors let alone our willingness to engage with change. Reflecting on current world events illustrates how change is managed within its context and the resources available, whether time, effort, money, collaboration or diplomacy.
Identifying the threshold of something new is, however, critical and brings with it energy and hope for something better. I try to use this when a patient and their family walk into clinic for the first time for a previously unmanaged long-term problem. “What would make this a good appointment and the start of you getting to grips with this?”
Well, 2024 could be that start of something new in lots of places. Half of the world’s population, I am told, is going to the polls this year with national elections in 16 countries in Africa, 9 in the Americas, 15 in Asia, 13 in Europe and 3 countries in Oceania, this will more than likely include the UK general election.
The Wales First Minister, Mark Drakeford, ended 2023 by announcing his resignation of Welsh Labour Leader and will step down as First Minister in March 2024 The hopeful candidates to replace Mark Drakeford have already outlined their priorities which have include NHS spending and NHS waiting times but the next First Minister will also need to answer the question, how do we improve child outcomes in Wales?
One well documented way of improving child outcomes is by getting kids back into school. This is known to be associated with improved life opportunity and better long-term health outcomes. I’ve written more about this in a previous blog.
However, improving pupil absence isn’t going to be easy. Education funding has declined from 5.7% of GDP in 2009/10 to 4.2% (2022/23), or a 6% drop in per capita expenditure in Wales. Fresh approaches should be included to address medically authorised absence, which accounts for 50% of persistent school absence, but is often overlooked. Dr Rowena Christmas, RCGP Cymru Wales Board Chair, has written on the role of the GP and both her and I have worked our way on to the new Welsh Government School Absence taskforce, to represent physical health, whether asthma, epilepsy, persistent pain and fatigue or other factors.
Please let me know of your ideas and practice.
Making sure children are back in the classroom is our number one priority. By working together we will ensure that all children and young people are given the best possible start in life and are supported to reach their potential.
We all in child health have a responsibility to maximise attendance and future life opportunity, health and wellbeing and I, in my role as RCPCH Officer for Wales, am linking with Public Health Wales, mental health practitioners and others and hope to hear of new ideas or existing programmes to share with the taskforce, so please let me know if you have any exciting opportunities and ideas that I could support and share with the Ministerial led taskforce.
We also know the best start to school is in the preparation for it. The first 1,000 days is critical but there appears to be a marked variation across health boards in terms of this best start, such as staffing by health visitors and continence nurses, waitlists, and outcomes such as oral health and healthy weight. What is more the 2022 School Readiness Survey indicates a deteriorating situation with 59 percent of teachers surveyed reporting higher or similar numbers of children with difficulties such as toileting, sleep, diet and eating as well as communication, emotional regulation and age appropriate sedentary behaviour.
Working Together to Give Every Baby & Child The Best Start in Life is one of the key strategies in a new approach taken on by Gwent services as the first Marmot Region in Wales (The Health Gap: The Challenge of an Unequal World: the argument - PMC. nih.gov). This echoes two of the 8 Marmot Principles - if you’ve not read it, The Health Gap is an accessible, highly rationale and compelling book by Michael Marmot - and is Gwent’s first step to becoming “a fairer, more equitable and inclusive” county (Gwent Marmot Region - Gwent Public Services Board Gwent Public Services Board. gwentpsb.org). Data shows a far greater proportion of children are living in poverty in Blaenau Gwent, 35.5%, Newport, 36.3% and Torfaen 34.4%, each associated with higher infant mortality and 20% shorter life expectancy compared to Monmouth and Wales as a whole.
Part of their plan is allied to “allocative value” and the need to rebalance resources across different groups to meet need. One specified challenge is to reallocate some resource from end of life to the beginning to head off the inequity in life expectancy. It will more than pay for itself in improved opportunity and tax receipts, but requires sensitivity and clarity of purpose backed by whole system and workforce planning from which we can learn.
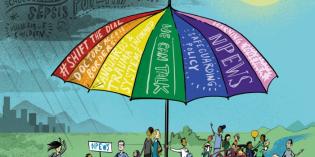
It also requires political support. The College, to this end, has published “Our manifesto for the next UK General Election – support children’s health and wellbeing in a changing world (2024)” calling to political parties to change the “machinery of government” to support better policy making for children and young people.
This means:
- establishing a cabinet level Minister for Children and Young People
- adopting a child health in all policies approach
- developing a cross-departmental Child Health and Wellbeing Strategy
And this circles back to Mark Drakeford’s resignation, not so much to mark out the end of an era but to start something new. The next First Minister will need to show they will be prioritising child health outcomes and ensuring children can thrive in Wales.
For now though I’m going to see if I can find my daughter’s secret stash of chocolate and wish you a happy New Year.
- Case Study
“What should I be doing? I just want my child to get the most out of school,” was the answer of a mother of a young child to the opening question “what do you hope for from this appointment?"
Her child had been referred for further assessment of short stature, “unusual appearances” on X-ray mild gross motor delay and prominent eyes. The child’s mother had been told of the likelihood of a genetic condition and had seemed to have come to terms with this. Other history identified the child had been a floppy baby and began to walk at 19 months but had otherwise developed normally. The child appeared bright and engaging, was just below the 0.4th centile for height, had a slightly laboured gait, strong facial features, small teeth and broad short fingers. Having already reviewed the child’s case as a team particular x-ray features such as acroosteolysis of the child’s fingertips, vertebral changes, low density bones and wide sutures and bony islands on the skull x-ray pointed to Hadju-Cheney Syndrome, a rare condition with known abnormalities in the NOTCH-2 gene.
We of course spent time talking about what this might mean to her child, and the limited benefit of medication and surgery. In keeping with the mother’s wishes our focus has remained throughout the child’s care on optimising independence, physical activity and normal family life whilst mindful of potential fracture risk. We have talked particularly about dental care and diet, given the risks from her condition, and helped to manage appointments and investigations to keep school loss to a minimum. We have enabled peer support, supported local therapists and our conversations with school, that included her mother and ultimately her older child, helps to agree simple strategies to empower everyone, avoid unnecessary assumptions about learning ability and safety and promote normal attendance and participation.
Is this not what all children with long term conditions need? And if so can we codesign generic systems of care and support to optimise attendance, and this start to life, without increasing the burden and expectation on teachers?