Paediatricians, who traditionally focus on physical health and child development, are broadening their remit to support and care for the mental health and well-being of children and young people. Paediatricians are now regularly encountering children with an array of mental health needs across health settings, including emergency departments.
These environments are often not designed to support children's mental health and almost half (46%) of children who attend A&E in a mental health crisis have to wait in the emergency department for over 48 hours before a suitable onward care plan is in place. Paediatricians are also seeing more children in their clinics who have mental health needs alongside their physical health problems. Access to specialist mental health services is challenging due to current demand but for many children and young people early recognition, advice, and signposting to other sources of mental health support through schools, primary care and voluntary organisations can be sufficient.
Paediatricians are not trained psychiatric professionals, so do not treat severe mental illness, but they have many of the skills needed to identify and respond to distress and common mental health problems in childhood and adolescence. The professional body, Royal College of Paediatrics and Child Health (RCPCH) has published an updated position statement which outlines the changing role for paediatricians in prevention, recognition and early intervention for poor mental health and advocates for clinicians to have improved access to further training and support where there are gaps in knowledge and/or confidence.
This change comes after an unprecedented rise in mental health problems for children and young people. Data across England now shows that:
- Almost one in five (18%) children aged 7-17 now has a probable mental disorder, a 50% increase from 2017.1
- Hospital admissions for children and young people with eating disorders have more than doubled in five years - going from 3,806 in 2016/17 to 7,904 in 2022/23.
- The number of open referrals to Children and Young People’s Mental Health Services is the highest on record with 496,897 referred to services in November 2023, an increase from 493,434 in October 2023.2
- Rates of self-harm remain high for young people, with almost a quarter (24%) of 17-year-olds self-harming each year. Suicide remains the leading cause of death for young people in the UK.3
Mental health services are doing their upmost to meet this rise in demand for treatment, but a lack of staff and resources means many young people are being placed on exceptionally long waiting lists. This can lead to their symptoms becoming more serious over time and eventually presenting to emergency departments and paediatric settings in crisis. RCPCH is calling for increased funding and capacity for community based mental health services so that children can access quality and timely support before reaching extreme distress.
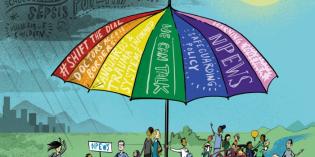
In the meantime, paediatricians are well placed alongside the rest of the children’s workforce (teachers, social workers, voluntary services) to support children’s mental health. This can include but is not limited to promoting positive mental health in all their interactions, early recognition of and intervention for common mental health problems, supporting effective joint working and integrated pathways with mental health services, and providing a safe environment for children in paediatric wards and emergency departments, by having appropriate staffing levels, and necessary training for managing acute distress.
RCPCH Officer for Mental Health, Dr Karen Street said:
The entire children’s workforce has a role to play in tackling the current crisis in children’s mental health, but as paediatricians we are particularly well placed to make a difference. Research shows paediatricians are the most trusted profession for secondary school children, across all ethnicities and backgrounds and that children see doctors as a key group to support their mental health.
We know that paediatric settings and emergency departments are not ideal for children and young people experiencing a crisis in their mental health, but they cannot be left without support. These vulnerable patients are all our patients, and we must work together to ensure they receive the right treatment, in the right place, at the right time. The paediatric profession is committed to holistic care for children and young people, which necessarily includes both their physical and mental health, and adapting to the changing challenges for children and young people to give our patients the best quality care and support - we now need Government to follow suit.
If we are ever to get out of this dire situation then we need meaningful support for health services and staff, as well as child focused polices that can improve the physical, emotional, social, and educational wellbeing of young people. The responsibility to tackle this growing mental health emergency cannot be left to healthcare professionals alone.
Chair of Royal College of Psychiatrists Child and Adolescent Faculty, Dr Elaine Lockhart, said:
We are aware as child and adolescent psychiatrists that our current specialist mental health services are not sufficiently resourced to meet the increased need of children and young people who are struggling with their mental health. Although our focus as psychiatrists must be on those we see in specialist mental health services, we fully support the work our paediatric colleagues bring to earlier identification and support of mental health difficulties in children seen within their services.
We also support their call for increased focus and funding of children’s mental health services so that there are well trained and resourced teams across the country who can meet the full spectrum of need from mild difficulties to severe mental illness.