For more on sustainable paediatric care, see Greener paediatrics
Why this toolkit matters
Climate change is the greatest health threat of the 21st century, and children are among the most vulnerable1. The NHS contributes around 4.4% of the UK’s carbon footprint, and paediatric services have a critical role in reducing emissions while improving care quality2.
This toolkit provides tools and strategies for paediatric services in acute or emergency care settings to deliver on the NHS commitment to NetZero. It provides practical steps, tools, and resources to help you embed sustainability into everyday practice without compromising patient safety or education. Every small change in a high-volume pathway can make a big difference.
What do we mean by greener paediatrics?
The integration of sustainable healthcare into everyday paediatric clinical practice, ensures that care is safe, effective, and supports the NHS ambition to reach Net Zero.
What is sustainable healthcare?
Sustainable healthcare meets the needs of our populations, without damaging the health or ability to meet the healthcare needs of vulnerable people now or in the future3.
Cutting emissions and achieving NetZero can fit into usual workplans without becoming a cost to patient safety, education, training and development. This toolkit is aligns with current models of working and aims to demonstrate how all paediatricians at any training stage have a role to play.
The Centre for Sustainable Healthcare has widely recognised four principles of sustainable healthcare3:
- Prevention: Promoting health and preventing disease by tackling the causes of illnesses and inequalities.
- Patient self-care: Empowering patients to take a greater role in managing their own health and healthcare
- Lean service delivery: streamlining care systems to minimise wasteful activities.
- Low carbon alternatives: Prioritising treatments and technologies with a lower environmental impact.
Similarly, in the context of clinical innovation, NHS have produced the STEPS to Low Carbon Care Delivery4:
- Settings: Reduce the carbon and resource intensity of care settings
- Treatments: Reduce the carbon emissions from treatments and deliver high quality care
- Efficiency: Right care right place, right time. Reduce inefficient and inappropriate care delivery
- Prevention: Reduce care needs and the burden of disease
- System change: Ensure net zero is embedded as business as usual
What can I do?
Prevention
Preventing illness early is one of the most effective ways to cut healthcare emissions.
Children’s services and paediatricians hold an important role ensuring that children have timely access to care, preventing health problems worsening and compounding into adult services.
The Academy of Medical Royal Colleges highlights that the most critical window for improving lifelong health is in childhood, starting from pregnancy5.
Indicators of child health include:
- Healthy weight
- Oral health
- Vaccinations
- Clean air
- Mental health
There needs to be a collaborative effort from the whole child health workforce with a commitment to promoting healthy behaviours in children and young people as well as using case histories to understand environmental health indicators, providing education and promoting equitable access to vaccinations.
- Resident tip
The College Progress+ curriculum includes capabilities in health promotion and illness prevention including curriculum learning outcome 5 in the core paediatrics training which states:
- Paediatricians must promote healthy behaviours in conversations with children, young people and their families/carers, from early years through to adulthood; taking into account the potential impact of cultural, social, religious and economic factors on the physical and mental health of children and families.6
Clinical pathways
Sustainable models of care must enhance, not compromise, quality.
Paediatricians are expected to contribute to improving healthcare services and there is real value in assessing outcomes alongside wider costs and impacts7.
In fact, many quality improvement projects already support sustainable healthcare by innovating clinical pathways to be more streamlined, effective and safe.
To do this well, you need:
- To utilise proven methods and develop practical skills which integrate sustainability into quality improvement projects.
- Strong collaboration across the multidisciplinary team, especially among consultants, nurses, and pharmacists, to enable meaningful action and urgent change.
By focusing on high volume pathways – a small change can have a big impact. Mapping clinical pathways and identifying the carbon hotspots can provide guidance for where to focus a change in your local area and pathways within your service. Again, centre for sustainable healthcare has some good resources.
Here are some tools you can use:
- Sus-Qi
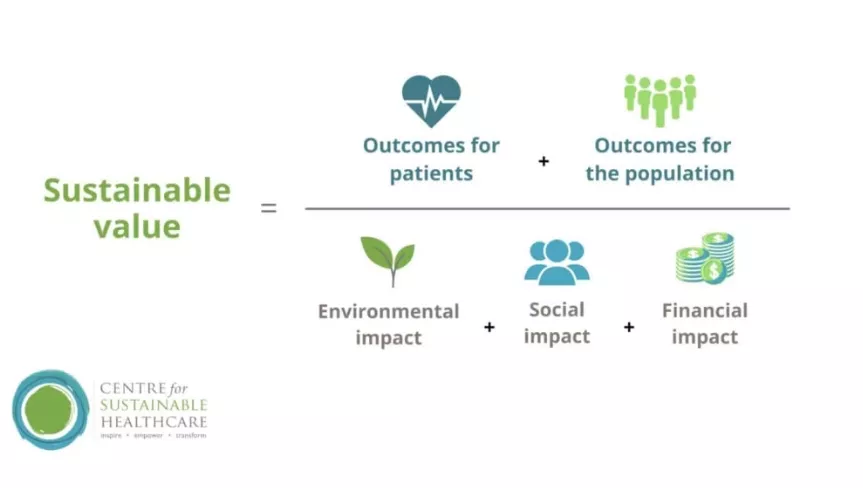
One method available is the Sus-QI method designed by the Centre for Sustainability8. It builds on quality improvement methodologies and involves measuring the value and quality of improvement projects using the triple bottom line:
- Lower carbon emissions or other environmental harms.
- Better patient, family and staff experiences.
- Cost savings.
- CPD courses
CSH sustainable child health - This course, developed in collaboration with the Royal College of Paediatrics and Child Health, explores the impacts of climate change and nature loss on the health and wellbeing of children and young people, and the ways in which the healthcare system is both vulnerable to and contributing to these crises. Using real world case studies, the course describes how we can deliver healthcare sustainably and adapt to climate change and explores what the wider benefits might be, outlining a comprehensive vision of a sustainable system of care that maximises children’s opportunities to thrive and supports the ecosystems they depend on to flourish.
Sustainability in Quality Improvement (SusQI) - This intensive course introduces health professionals and educators to the concept of ‘sustainable value’ and the ‘SusQI’ framework for integrating sustainability into quality improvement. Learning from real examples, participants explore in depth how the framework can be applied in practice to develop preventative, holistic, lean, low carbon, high quality care.
CSH Carbon footprinting for healthcare - This course is designed to help healthcare professionals, quality improvement leads, managers and healthcare students gain an understanding of what a carbon footprint is, what a life cycle analysis is, how it is measured and how it can be used in the efforts to reach net zero. We will also explore existing carbon footprinting studies in healthcare and what can be learned from them.
- Medicines database
Healthcare LCA (Life Cycle Assessment) database - an up-to-date open access database of published lifecycle assessments within healthcare. The database makes it easy to search for the carbon footprints of specific procedures, services and equipment.
CYP and family engagement
Children and young people (CYP) must be at the heart of service design and improvement.
Using CYP engagement methodologies helps ensure that child health services truly reflect their needs and priorities. CYP not only care about reducing the environmental impact of their care, but they also have valuable ideas about how services can work better for them9.
When improving services locally, meaningful engagement means creating real opportunities for CYP to share their views and influence decisions that affect them. Our CYP Engagement Team offers practical resources to support you in doing this well10. In 2026, we will publish new engagement standards to help ensure that every project hears from a diverse range of voices.
- What do children and young people say?
- They want clinicians to talk openly about climate change and health.
- They worry about waste in healthcare (e.g., single-use plastics in medication packaging).
- They want to be part of the solution and share ideas for greener care.
- Climate anxiety is real and impacts mental health—sustainable practice can help alleviate this.
Knowledge exchange
Working collaboratively and sharing best practice is essential.
As the NHS accelerates its journey to Net Zero, there is a real risk of duplication and services working in isolation on similar projects without sharing learning. Given the urgency and scale of change required, collaboration is essential. We need to share best practice, amplify what works, and spread ideas beyond sustainability networks.
Paediatrics is a diverse specialty, making a “one size fits all” approach unrealistic. However, many successful initiatives from adult care can be adapted for children’s services with only minor adjustments. By learning from others and sharing your own work, we can move faster and achieve more together.
- How and where to share your projects
- Submitting projects to conferences and journals
- Share projects on the CSH green paediatrics network
- Green clinical networks within your trust
- Submitting case studies to RCPCH
- 1
See https://www.rcpch.ac.uk/resources/impact-climate-change-global-child-he…
- 2Pencheon D, Wight J. Making healthcare and health systems net zero. BMJ. 2020 Mar 30;m970.
- 3
See https://sustainablehealthcare.org.uk/about/our-story/the-principles-of-…
- 3
See https://sustainablehealthcare.org.uk/about/our-story/the-principles-of-…
- 4
See https://sbrihealthcare.co.uk/competitions/guidance-for-applicants/steps…
- 5
See https://www.aomrc.org.uk/wp-content/uploads/2023/09/Securing_our_health…
- 6
See https://www.rcpch.ac.uk/resources/rcpch-progress-plus-curriculum-syllab…;
- 7
See https://www.rcpch.ac.uk/resources/rcpch-progress-plus-curriculum-syllabi
- 8
See https://sustainablehealthcare.org.uk/sustainable-quality-improvement-su…
- 9
See https://www.rcpch.ac.uk/resources/preserving-the-world-for-future-gener…;
- 10
See https://www.rcpch.ac.uk/resources/engaging-children-young-people









