The Darzi review has recommended greater investment in children's services, yet the NHS Wales overspend is £385 million1 and we are told there is no money - how is this circle squared for children and young people's healthcare in Wales?
A budget doesn't limit freedom, it creates it.
This overspend is despite a cash uplift of £744 million and a saving of £210 million in a system that was allocated £10.6 billion in 2023-242 . So what are the alternatives to borrowing ever greater amounts? One is to better redeploy funding and resources around the system.
In a recent University Hospital of Wales (UHW) corridor conversation, a senior paediatrician, frustrated by a lack of funds for unmet need, argued that current specialist allocations were no longer needed in a particular area - the activity now being absorbed by secondary care. "If there was effective oversight this would not happen," he said, essentially describing the challenge of stewardship as a solution to "a tragedy of the commons"3 4 as discussed by Wilson et al. In their 2020 paper5 they start from the economic viewpoint of a shepherd who adds more animals to common grazing land. This encourages others to do the same and ultimately depletes or destroys the primary resource.
Stewardship at a whole system level
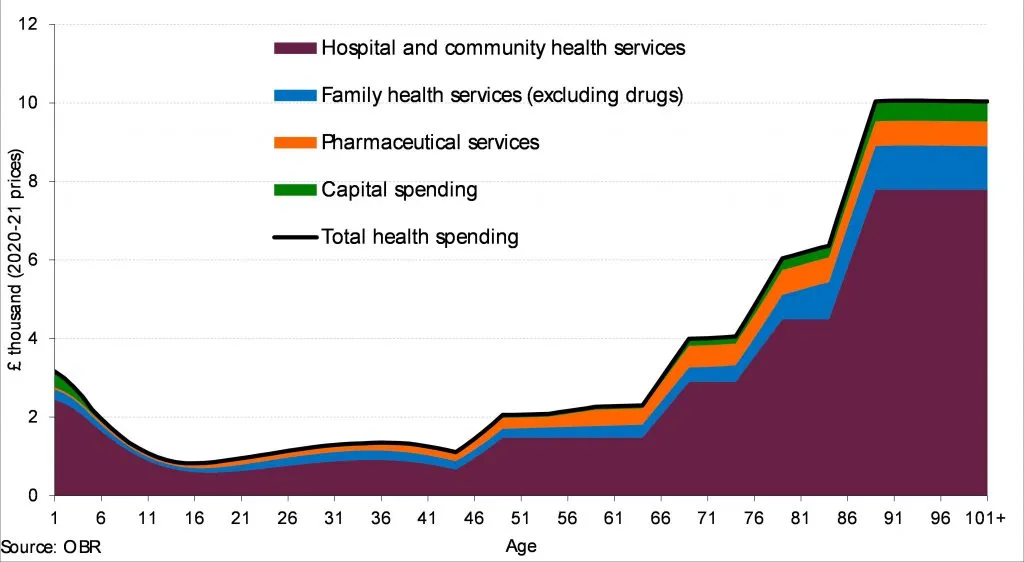
So with this in mind, acknowledging every budget is tight and demand is ever increasing, how about we go ahead and top slice 3% from an area of great expenditure, say for adults 65 years old and over (see graph above showing age as a driver of health spending) and redeploy for redesigning care for children and young people - in turn reducing costs of future elderly care6 . Three percent - just over recent inflation - is not insignificant, but pales in comparison to the projected 106% growth in cost of care for the elderly over the next 15 years7 . Yet 3% from the 65 years+ budget (over 40% of the total budget of NHS Wales) amounts to redirecting £130 million to the £600 million budget for those under 16 years old in Wales8 - an increase of approximately 20%.
This is not without precedent - top slicing occurred for mental health in ABUHB (Aneurin Bevan University Health Board) to greatly improve early intervention for young people and provide a bridge with physical health.
The yield of stewardship at service and health board levels
Stewardship can be delivered at all other levels of healthcare too, including by individual services, paediatricians and their teams. In last month's blog, I mentioned how a different model of funding was used to incentivise change9 . My service in Oxford was switched to a bundled tariff that recognised the individual importance of therapy and nursing staff for the one stop model and our interdisciplinary care. This improved joint decision making, empowered patients, enhanced networked care and minimised redundancy.
As a result, we found we yielded time and resource to redirect to populations with unmet needs including those with persistent pain, skeletal dysplasia or problems related to sport and exercise.
I retested the Oxford tariff and model to greater effect in London and the South East, as shown in the independently audited BSR (British Society for Rheumatology) best practice programme 202210 . Using a combination of data sources (NHSE specialist dashboard (SSQD), hospital episode statistics (HES), local activity data, BSR and NRAS workforce surveys) we were able to show rapid growth and diversification over five years to build two services (rheumatology and pain), each comparable in patient referral rates (and complexity) to any of the largest national centres, but with less than a third of the staffing costs.
What's more, the funding model, together with a benefactor's endowment, contributed to a balance sheet surplus of £3 million over five years. This is where stewardship falls down. At the hospital and health board level, as Wes Streeting has recently indicated, budgets become murky with little data transparency. How we use this data and resource should be a collective decision11 - scale the model or flip to fund similar innovation elsewhere - but using it to create the UK Government's league tables may miss the point.
Stewardship in Wales
In Wales, things are different and offer other opportunities and challenges. Paediatric rheumatology is funded by a whole service model. This too has allowed reallocation of resource and is now being used to develop a new integrated funding model to best support the large population with persistent pain.
This was initiated with support of WHSSC (now JCC, or NHS Wales Joint Commissioning Committee) who recognises the role of stewardship. In its five-year review in 2022, a very clear analysis of funding of all specialist services showed that up to 50% followed a clinical activity across to NHSE. This has spurred many stewardship discussions, including repatriation of activity, which can hopefully be resolved with support of both the Child Health Strategic Network and health boards.
Another challenge is to steward funds divided across the other 12 national networks, each charged with a life course approach that is system or condition specific (eg cancer or diabetes). In a report at the recent Welsh Paediatric Society clinical meeting, the strategic child health clinical network shared that only one network had a CYP plan and it was not clear whether a well-defined budget existed.
This is similar for paediatric therapy. Two years ago the need for a gap analysis for child health services was identified but planning has yet to begin.
A summary of solutions
The need for stewardship is clear and specific commitments to this have been identified above - accountable leadership, clear boundaries for children and young people's services, transparent data and whole system budgets, the right for children's services to organise themselves at national and local levels. But further elaboration can be found in the paper by Wilson et al5 . In particular, we need an empowered Child Health Strategic Network (and health boards) to lead on this, hold the other networks accountable and engage all paediatricians in repatriating activity, participating in stewardship and contributing to the development of an effective plan for spending an additional £115 million.
We at RCPCH Wales want to help, so if you haven't yet, please complete the RCPCH Wales survey and read the College's blueprint for transforming child health services.
- Case study
-
This is a composite case of several young people with similar problems and management.
A 12-year old boy with juvenile arthritis has swollen, restricted wrists affecting his hand function. No other joints are involved. His difficulties include buttons and dressing, turning taps, holding heavy objects and in particular effects on his handwriting and school performance. An OT has provided school guidance and supportive aids, but refractory inflammation underlies this.
Although conventional assessment does not score the right number of joints recommended by NICE guidelines, he has been prescribed a biologic medication without significant benefit. Methotrexate and similar drugs have not been effective. New alternative biologics cost £4,000-25,000 per annum.What should the paediatric rheumatologist do?
- Stop biologic treatment because ineffective and the funding guidelines are not met leaving the partial effect of steroids and NSAIDs
- Follow the above and add conventional disease modifying drugs in the hope they may now work
- Try the cheapest alternative biologic (knowing the risk-benefit of each is indistinguishable)
- Present information on each biologic to allow patient and family choice irrespective of cost
- Refer to someone else
What would you do if there was a tightly controlled drug budget for your population of patients meaning a decision for one patient has a potential impact on another? What if the cost is devolved to a Health Board, in keeping with potential budgetary changes?
- 1www.wao.gov.uk/news/all-health-boards-breach-break-even-duty-amid-deepening-financial-pressures
- 2www.wao.gov.uk/news/all-health-boards-breach-break-even-duty-amid-deepening-financial-pressures
- 3en.wikipedia.org/wiki/Tragedy_of_the_commons
- 4Hardin, G (1968). "The Tragedy of the Commons". Science. 162 (3859): 1243–1248
- 5 a b https://journals.sagepub.com/doi/full/10.1177/0141076820913421
- 6Marmot - The Health Gap; improving health in an unequal world, 2017
- 7www.lse.ac.uk/cpec/assets/documents/cpec-working-paper-7.pdf
- 8cms.barnardos.org.uk/sites/default/files/2023-11/UK%20public%20spending%20on%20babies%2C%20children%2C%20and%20young%20people%20-%20Alma%20Economics%20-Nov%2023.pdf
- 9www.rcpch.ac.uk/news-events/news/silver-slipper-two-new-champions-child-health
- 10www.rheumatology.org.uk/news/details/Best-Practice-Awards-shortlist-announced
- 11journals.sagepub.com/doi/full/10.1177/0141076820913421