Data and insights
In this section, we look at trends in flexible working across the the last 10 years (as of 2025) for postgraduate doctors in training (PGDiT) and the last five years for consultants and SAS doctors.
These are publicly available and sourced from NHS England, NHS Education for Scotland, StatsWales and the General Medical Council (GMC). Further information on staff working patterns for England and Wales was retrieved via Freedom of Information requests.
Data for PGDiT
The charts below display the number of PGDiT in Paediatrics according to the GMC Data Explorer, and the respondents to the GMC National Training Survey and percentage training less than full time, according to the GMC Education Data Tool.
Flexible working more than doubled from 2015 to 2025. At the start of this period numbers were relatively stable at around a quarter of PGDiTs working less than full time from 2015 to 2018, but this since increased quite dramatically post-pandemic going from 30.8% in 2019 to over half by 2023 and reaching 59.7% in 2025.
The below chart displays PGDiTs and flexible working patterns for each nation from 2019 to 2025, as reported by the GMC NTS. For England, Scotland and Wales, there was a significant increase in those working less than full time. In England, for example, numbers essentially doubled from 31.8% in 2019 to 61.6% in 2025 with similar trends in Scotland (26.6% to 47%), Wales (22.9% to 58.5%) and Northern Ireland (16.7% to 36.7%).
When looking across each training year, there was an annual increase in flexible working from 2019 to 2025 for most training levels.
Data for consultants
As shown in the below chart, the headcount of paediatric consultants in England increased year on year from 3,980 to 4,603 (15.7%) with a similar increase in Wales of 14.6%; in Scotland the increase was significantly less at 8.5%. In England, consultants working flexibly increased from 28.1% to 34.2% and Wales saw a significant increase to 33.6%, a third of the headcount; Scotland on the other hand remained relatively stable.
The chart below displays headcount consultants working flexibly by NHS Region in England and Health Board for Scotland and Wales. NHS Western Isles and NHS Shetland were omitted due to small numbers.
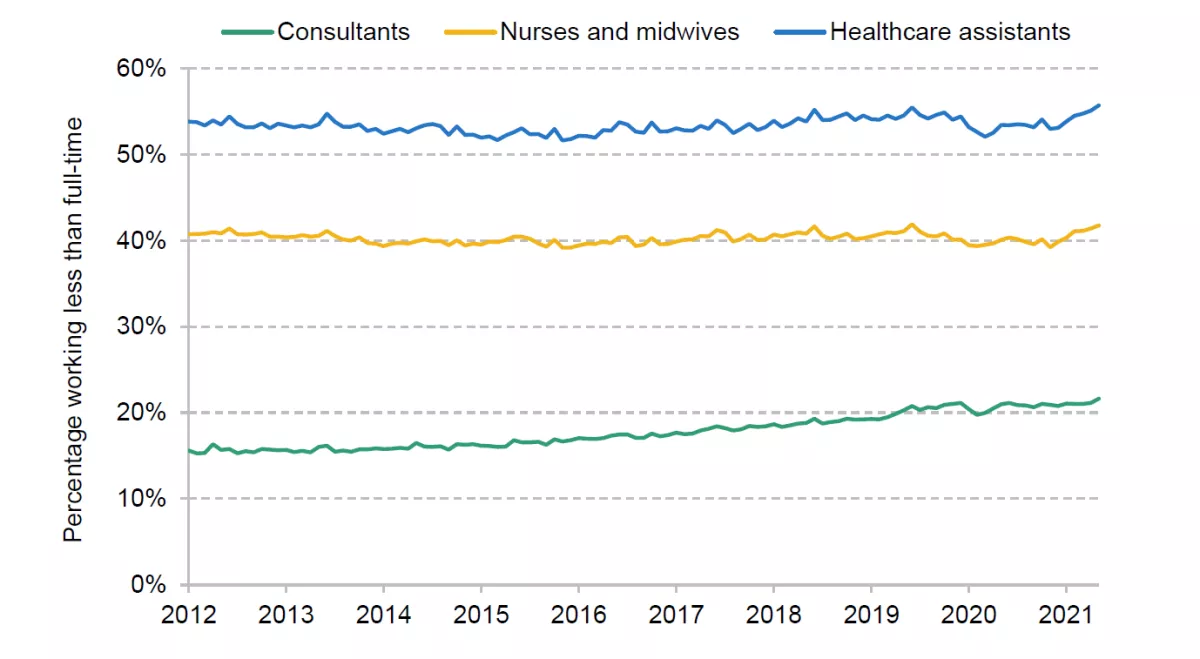
A 2023 study by the Institute of Fiscal Studies investigated the patterns of LTFT Consultants working in England across all specialties. Overall, the proportion of consultants working LTFT increased from 15.6% in Apr 2012 to 21.6% in Aug 2021, as shown in this chart (IFS, 2023, p8).
The changing age and gender of the paediatric workforce explains almost half of the increase in LTFT working from 2012 to 2021. While female consultants are more likely to work LTFT, this difference narrows with age. Around 30% of female consultants under 60 work LTFT compared to 10% of male consultants, but at 60-64 years, the gap closes significantly with 34% of male consultants and 45% of female consultants working LTFT (IFS, 2023, p13).
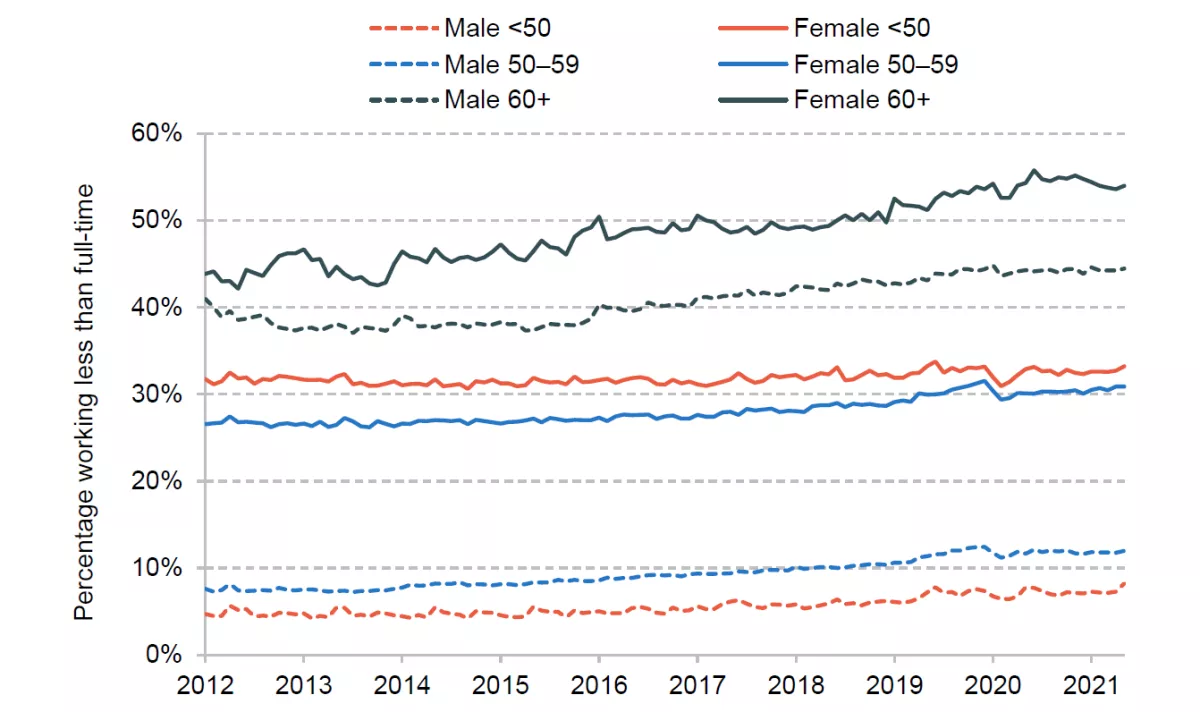
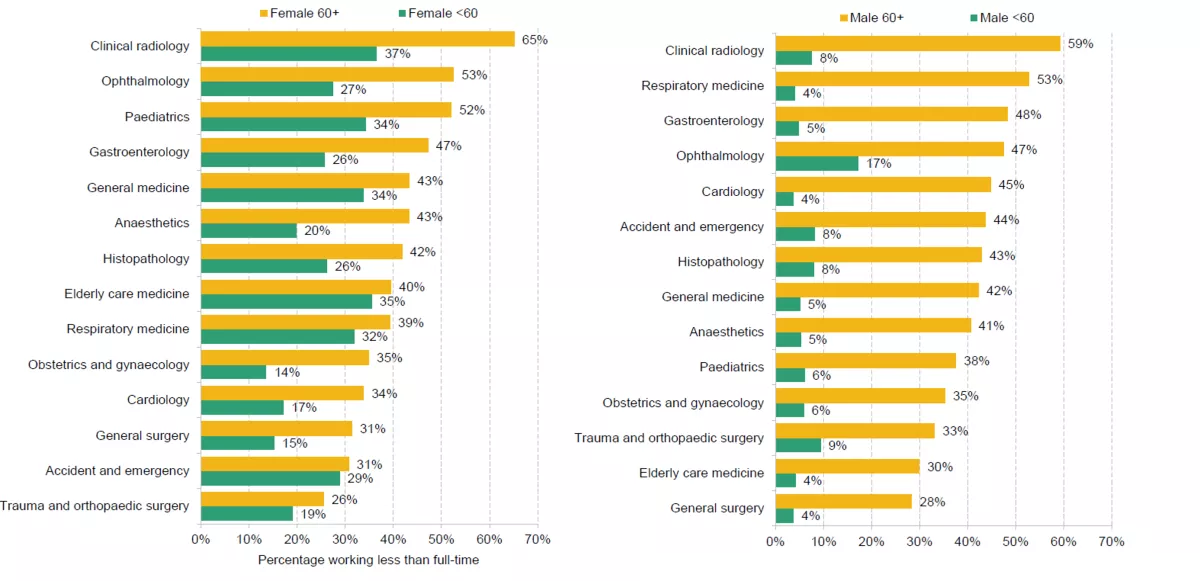
Consultants often shift to LTFT before exiting the NHS. Four years before leaving 24% work LTFT which increases to 39% two years prior and then 51% one year before. When looking at working patterns by specialty, paediatrics has the third highest proportion working LTFT once adjusted for age, gender and trust composition. This is largely driven by female consultants with the third highest in both the over 60 group at 57% and under 60 group at 34% (IFS, 2023, pp 14-16).
Data for SAS doctors
The headcount of SAS doctors in England increased by 14% but remained relatively stable for Scotland over the five-year period. For both nations the proportion working flexibly remained stable at a consistent 37-38% in England and 60% in Scotland. For Wales, data were not sufficient to explore working patterns.
Legislation
Key legislation relating to flexible working
- Work and Families Act 2006
- Equality Act 2010
- Children and Families Act 2014
- Employment Relations (Flexible Working) Act 2023 - permitted two statutory flexible working requests every year, set a two-month time limit for dealing with requests; employers must consult an employee before refusing a request
- Flexible Working (Amendment) Regulations 2023 - removed the need for employees to have at least 26 weeks' continuous service, before making a flexible working application
Also see general government advice on part time workers' rights.
Other legislation relating to flexible working in NHS
- British Medical Association
-
With expectations of work and work-life balance changing, the NHS understands flexible working opportunities are key to attracting and retaining talent. Discussions around flexible working should form part of wider conversations on individual wellbeing while employment models and shift patterns need to evolve to accommodate flexible working.
In 2003, there was agreement between the BMA, Department of Health and NHS Confederation in England:
- encourage flexibility on part of employers as an aid to recruitment and retention of doctors with other commitments
- ensure that part-time doctors do not suffer direct or indirect discrimination
- ensure that part-time doctors are able to keep up to date and continue their personal development
- avoid penalising employers who recognise the need for flexible working arrangements and the needs of those employees wishing to work part-time.
- NHS Improving Working Lives initiative 2000
-
This initiative placed an expectation on all NHS employers to promote a healthy work-life balance via flexible working arrangements, access to work-related health services and the right to request flexible working.
As part of this initiative, the NHS Flexible Careers Scheme (FCS) allows for doctors to move in and out of full-time and part-time working, to spread training over a longer period, reorganise hours, take career breaks and wind down gradually before retirement or return to the NHS. Doctors wishing to work 50% or more as part of a job share or just under the flexible working ruling can apply for any substantive post. For those working less than 50% the FCS provides central funding to support this.
- NHS People’s Plan, 2020-21
-
This stipulates that all employers are required to be open to all permanent roles being flexible and that they should be advertised as such. Conversations around flexible working should be normalised and included as standard during inductions and appraisals. Flexibility should not require justification and should be offered as far as possible.
This change in ways of working is supported by guidance for both individual and managers, including:
- offering the opportunity for regular conversations to discuss flexible working options
- offering flexible working from the beginning of the role
- supporting individuals, managers and teams to work together to explore flexible working options
- engaging with opportunities to consider flexible working options for every job and clearly communicate these to staff.
See NHS England flexible working toolkit for individuals and managers
- NHS terms and conditions of service
-
The NHS Terms and Conditions of Service (TCS) handbook was updated in September 2021 to allow for the right to request flexible working from day one - two years in advance of the universal statutory requirements.
- NHS Long Term Workforce Plan 2023
-
This highlights the importance of flexible working in attracting and retaining staff with an ambition to go beyond statutory requirements in terms of flexible working. Organisations and systems are encouraged to consider these principles and, where possible, support individuals, managers and teams to work together to explore the flexible working options available.
Guidance introduction
The NHS encourages flexible working for all its staff has recognised that when it comes to working doctors and postgraduate doctors in training (PGDiT) there has been a shift in expectations with traditional linear career models declining in favour of portfolio working and employment mobility.
To support these ways of working the NHS developed a framework that informs flexible career pathways. Doctors may choose to train less than full time (LTFT) because of childcare or other caring responsibilities, personal physical or mental health issues, or commitments outside of medicine (national or international sport or religious roles, for instance), or simply because of wanting a different work-life balance. In this case, LTFT simply means reducing working hours to below 100% full time (40 hours per week) to a lower percentage, usually 60% or 80%.
Following a period of flexible working, any member of staff has the right to return to their role under their original contract at the end of the agreed period and on no less favourable terms and conditions. See our returning to work guidance.
Guidance for PGDiT
As part of the employment legislation and NHS directive around flexible working detailed above, PGDiTs are entitled to apply for less than full time training with all requests considered regardless of reason. For more information, see our rota guidance for PGDiT (England).
- Making a request for flexible working
-
Requests can be made at the start of training or any time after being accepted on the training pathway. A minimum of sixteen weeks’ notice is required whether the request is prior to starting training or as part of a change during a training placement. However, PGDiTs should also follow local ‘deanery’ guidance, which in some cases may be longer to to allow adequate notification period for the employer.
Processes differ according to nation.
- In England, application is via the deanery with both TPD (Training Programme Director) and education supervisor informed of any changes in working pattern.
- In Wales, the process is centralised and any requests handled by Health Education and Improvement Wales.
- In Scotland, PGDiTs should discuss requests with TPD and meet with the local Associate Dean who will take any requests to the local educational supervisor.
- In Northern Ireland, the process is centralised at the Northern Ireland Medical and Dental Training Agency with requests sent to Heads of School. Approval will normally be given for the duration of a placement with rota templates completed and checked by HR and reviewed annually. For any changes - for example, returning to full time no applications should be made to the deanery in line with the 16-week deadline or according to local guidance.
PGDiT with Skilled Worker/Tier 2 Sponsorship are required to complete an NHS Sponsorship Reporting Form prior to commencing flexible working as any changes in working hours or salary must be reported to the Home Office. It is the Postgraduate Doctors in Training responsibility to liaise with the Local Office and UK Visas and Immigration (UKVI) to ensure that any proposed reduction in working pattern does not compromise your visa requirements. If on a Tier 2 visa, a change of employment application must be submitted to the UK Border Agency.
- Working patterns
-
Flexible training posts are usually only approved if over 50% for educational purposes, but it is possible to work at a lower percentage in special circumstances for a limited amount of time. Shifts and hours are pro-rated as mentioned in the Gold Guide, but other arrangements are possible in cases of occupational health recommendations, particularly challenging caring responsibilities, or when breastfeeding a young infant less than one year of age.
Flexible training can occur as a slot share where two doctors share a single full time (FT) slot; this often equates to 120% e.g. two PGDiT at 60%. More complex arrangements are possible with negotiation. In cases, where a slot share is not possible the remainder of the slot remains unfilled. Supernumerary is also an option, but this is relatively rare given the option to slot share.
There is a contractual entitlement to a fixed working day pattern wherever possible with no shifts rostered on non-working days (unless otherwise negotiated). Between different jobs, it is not always possible to preserve the same working day pattern because educational opportunities, supervision and the needs of the department and PGDiTs can vary, but adequate notice should be provided.
- Annual Review of Competency Progression (ARCP)
-
ARCP is measured at the training percentage with the CCT (Certificate of Completion of Training) timeframe extended pro rata - unless negotiated and planned in advance with the educational supervisor. PGDiT with flexible working patterns will be expected to demonstrate capabilities relevant to their stage of training as described in their relevant curriculum.
ARCP assessments should occur no less than annually but at intervals of no more than 15 months, with any extension on a pro rata basis. Acting up as a consultant is pro-rated for the fixed three-month period within one year of anticipated CCT. The six-month grace period post training completion is not pro-rated.
- Leave arrangements
-
Annual leave and bank holidays are pro-rated regardless of days of the week worked. Study leave is also pro-rated except in cases of specific training courses required by the curriculum and can exceed pro rata entitlement. LTFT PGDiT should receive equitable access to study leave and funding, which is now centralised.
Guidance for consultants and SAS doctors
- Contract terms and conditions
-
All flexible working arrangements are documented in the Consultant Contract Terms and Conditions 2003 and SAS contract (2021 version for England, Northern Ireland and Wales, 2022 version for Scotland). These documents are updated routinely and as of 2022 all consultants and SAS doctors are entitled to request to work flexibly regardless of reason.
- Professional activities
-
Flexibility can relate to both timing and location of professional activities (PA) and employers must make reasonable attempts to accommodate requests, allowing doctors to return to a regular pattern of work when required (see BMA guidance).
Requests should be expressed in terms of the annual equivalent of the working week with any variations adjusted within the job plan. Part-time contracts can range from between one to nine PAs. This should not exceed six PAs for private practice. As a ratio of Direct Clinical Care (DCC) to Supporting Professional Activities (SPA), part-time doctors will require proportionally more SPA time to achieve CPD, undertake all teaching, audit, and clinical governance activities.
There should be no additional NHS commitment unless reflected in job planning and work needed to fulfil duties and responsibilities will be based on the agreed DCC. Part-time consultants wishing to undertake remunerated clinical work outside the main contract are expected to offer up to one extra PA on top of their normal working week.
For out of hours, part-time doctors will receive the full value of the on-call availability supplement. If on a different basis, they will receive the same supplement as a full-time consultant on an equivalent rota and if on-call on a day that they do not normally work, TOIL (Time Off In Lieu) or additional payment will be agreed.
Real life experiences
We gathered experiences from clinicians who have embraced flexible working patterns. Learn how they’ve balanced professional responsibilities with personal commitments and wellbeing.
Navigating clinical life and aspirations
From balancing clinical duties with personal life, to pursuing academic growth and to exploring paediatric sub-specialties, these stories offer valuable insights and guidance for anyone shaping their own career path.
- Balancing clinical practice and personal life
-
"I am a consultant community paediatrician and also a mother of two sons who have also chosen a career in medicine. I work full time in NHS Grampian but also deliver community clinics in Orkney as part of SLA. I generally do not have out of ours commitments and recently started to have a compressed week working four days per week (it was possible as my Orkney work is delivered at non specified time).
"Having the flexibility in my work with no out of ours commitments and later working four days per week has certainly created the right work life balance for me. My boys didn't miss out in any extracurricular activities and have viewed working in medicine positively and have chosen it as a career .I have been able to volunteer acting as a clinical adviser for the RCPCH Workforce Planning Board and have a lead CSAC role for my specialty in this region; all roles being quite satisfying. I have also been able to do voluntary work in the community. As I am approaching the end of my career, I feel really satisfied with my life both at work and out with and this could have not been achieved if I have been denied this flexibility."
Dr Hanan Hamed, Consultant Community Paediatrician
- Academic growth and career development in a sub-specialty
-
"I currently work as Consultant Paediatrician with special interest in diabetes. I worked flexibly at 60% for 6 years during training which helped me spend time with my children during a crucial part of their life and maintain better work-life balance. It also provided me with the opportunity to do projects, write papers and complete my MSc in Paediatric diabetes. One of the negative aspects of flexible working was that sometimes I did my project/academic work during my non-working days but it helped me develop mu skills in non-clinical areas and significantly enhanced my CV.
"When I started my consultant job, I started as full time, which was good initially. But as I started taking on more roles like college tutor and subsequently as Training Programme Director, it was difficult to manage a full time acute paediatric job. So in discussion with my clinical director who was very supportive, I dropped my direct clinical care hours to flexible working.
"At present, I share my ward/acute cover with another colleague who is also able to undertake other deanery roles like TPD. I undertake other roles like paediatric diabetes lead for my unit, teaching programme lead within my department, curriculum training programme director for specialty paediatrics and clinical representative within the Workforce Planning Board at RCPCH.
"These roles give me a good balance of direct clinical care and leadership/management experience with great satisfaction. This also helps me maintain a better work-life balance."
Dr Usha Niranjan, Consultant Paediatrician
- Building a career in paediatric Neurology and rare disease research
-
"I am working as a Paediatric Neurology GRID ST6 resident at the Bristol Royal Hospital for Children at 0.6 full time equivalent (FTE), and I am also employed as a clinical research fellow by the University of Bristol at 0.2 FTE currently. I was previously working as an academic clinical lecturer in Paediatrics, employed by the University of Cambridge and East Suffolk and North Essex NHS Foundation Trust, working 0.8 FTE while splitting my time between clinical and research roles. These roles have meant that I spend ‘own time’ keeping my mandatory training in various organizations up-to-date; complete a lot of paperwork including ePortfolio competencies; meet with supervisors regularly in clinical and research settings; and carve out a clinical research career that will enable me to work independently as a clinician caring for children with rare diseases while improving diagnostic pathways for them through my research. So why do it?
"I developed my passion for research in rare diseases early, as a 4th year medical student trying to understand what had caused my late cousin’s rare mitochondrial disease syndrome that caused her early demise. I was extremely fortunate to be studying at the same university that housed one of the largest international research groups for mitochondrial diseases. The experience of the PhD, under the guidance of Sir Prof Turnbull and Prof Taylor, became a deciding factor in my career trajectory. Despite starting in pure clinical training after the MBBS PhD in 2013, I continued to search for research opportunities because of the desire to improve understanding in mitochondrial diseases and other rare neurogenetic conditions. I then started my NIHR-funded academic clinical fellowship in the East of England, establishing collaborative networks and great working relationships with international experts.
"This three- year post, however, only gave me nine months in full time research, and so the search continued for ongoing clinical research posts, at which point I was awarded a locally funded clinical lectureship to continue the neurogenetic research theme while engaging underserved communities. However, this post did not have the capacity to include sub-specialty training, and therefore I am now working in Bristol in a Paediatric Neurology subspecialty training job while balancing a new clinical research fellow role funded by the Elizabeth Blackwell Institute – learning the ropes in a new deanery.
"How is that ‘balance’ going?
"Anyone who knows me will say the balance doesn’t exist. This comes with the territory of seeking funding opportunities, while trying to complete research projects, write papers, and train in a clinically demanding subspecialty! However, I am incredibly lucky to have an understanding husband who provides all necessary snacks for the late nights spent creating grant proposals. I also count myself very lucky to be working with a supervisor who happens to be an international expert in rare neurogenetic conditions and therefore understands what the juggle of clinical-academia entails in the field of paediatrics.
"How does flexible working look?
"This is very dependent on how your clinical rota is structured. We have ‘self-rostering’ in my Trust, which means I can choose to have a string of out-of-hour shifts that leaves me with several days without clinical shifts to focus on academic work. I am careful not to let the research work encroach on clinical time, and vice versa – but this means having to complete my clinic letters in a short timeframe to make sure things do not overhang. I have experience of working ‘blocks of time’ where I have been on pure academic work without clinical shifts, but this has left me feeling less confident in my clinical skills at times, therefore, I find working 1 week on – 1 week off, or having a few consecutive days of a particular role, helps my mind feel as settled as possible between the roles. This also means that working from home on my academic days lets me finish work on time to see the children! This is the underappreciated aspect of my work-life schedule – the value I place on being available at home as soon as work is finished in the ‘working hours’. It is a very special privilege to be able to work in this format, and so the hunt for ongoing funding continues!"
Dr Thiloka Ratnaike, Clinical Research Fellow and Paediatric Neurology Registrar
Balancing career and wellbeing
These stories offer personal reflections within their career. For more to support your journey and wellbeing, visit our Thrive Resource Hub (on RCPCH Learning).
- Rediscovering joy in medicine while balancing parenthood
-
"I was an SHO in 1997 working 72 hours per week and pregnant with my first child. The life changer of becoming a mum seemed incompatible with the long hours I was working and although I loved my job and had worked hard to get to that position I seriously considered a complete career change to something outside of medicine. I was very fortunate to have a supportive consultant who happened to be the LTFT adviser at the deanery - I remember the day she said “have you thought about going part-time?” and suddenly everything fell into place. I had never come across a part-time doctor- I didn’t know it was even possible. I remain grateful to her for kindness.
"I enjoyed 10 years of training LTFT as a registrar. 'Best of both worlds; my mother-in-law would say about my life as a working mother. I often found going to work a break from the frenetic life of being a mother! I enjoyed my time with the children but also found fulfilment in my purpose as a doctor. As an NHS doctor I realised how lucky I was as I saw many friends who worked in the private sector unable to continue their careers part-time.
"As a consultant I became full time partly for financial reasons but also to ensure my availability to do things /give advice when needed. When LTFT I often found myself working on days off so felt ready to commit more to work although I did and still do miss my days off and the balance it brought to the work- life conundrum. For a time due to shifts as a consultant 10 PAs meant a day off per week which suited me well when my fourth child arrived.
"Now as an older consultant in my twilight career years: I consider going LTFT in the next few years possibly as part of the partial retirement scheme to be able to spend more time with grandchildren if and when the fun starts again. Or maybe just to have some fun for myself outside work and family - now there’s a thought!"
Dr Rosemary Belderbos, Consultant Community paediatrician
- Championing IMG representation and wellbeing
-
"I am currently an ST7 paediatric oncology grid trainee in London, and I work 80% less than full time to support my various volunteering activities. When I moved to the UK in 2017, my first few jobs in the NHS were full-time placements, including my ST4-5 training years, after I joined training at ST4 level in 2021. I opted to work full-time as I wanted to achieve the competencies within a desired timeframe, and I was by myself in the UK without other commitments. Previously there were restrictions on minimum work hours for IMG doctors who are on a work permit visa, due to the minimum salary threshold. However, this was relaxed significantly after the pandemic when there was a growing recognition of the importance of well-being and contribution of overseas doctors to the workforce. Now, more number of doctors on work visa, both in training and trust grade doctors, are opting to work LTFT.
"My initial experience of volunteering started with Team Soft Landing to support and mentor other IMG (International Medical Graduate) doctors. I am also part of the organising committees for regional resident-doctor led MRCPCH teaching and research networks and volunteer as trainee representatives on the workforce planning board and international child health board within the college. Jobs related to these roles were mostly undertaken in my free time. Alongside developing my leadership, teaching and management skills, there was immense satisfaction from being able to support colleagues and advocate for IMG doctors within the wider organisation.
"Working less than full time since starting my sub-speciality training has given me the opportunity to continue with my volunteering roles without significant burn out. With a dedicated non-working day in the week, I can now schedule meetings, and mentoring / teaching sessions at fixed times with less need for last-minute re-scheduling. Flexibility with the non-working day also provides me opportunities to swap shifts and attend professional meetings within working hours.
"Flexible working in training allows for time to commit to volunteering work which for me has been a rewarding experience. Alongside providing me with essential non-clinical skills in leadership, teaching and management, it has given me the sense of being part of the wider paediatric community and develop meaning connections at work and beyond. I would hope employers, and educational supervisors facilitate the provision of flexible working for IMG doctors and doctors themselves should also consider this while working on their job plans and career progression. Innovative solutions to address rota gaps due to flexible work are a need of the hour for a sustainable workforce."
Dr Neelakshi Ghosh, Paediatric Oncology Doctor
- Job shares: collaborative approach to sustainable working
-
"I have been doing part time working for almost 12 years. It all started due to health reasons and childcare for my colleague. It started as job share and now we both work part time . The way it works for us is ward cover and attending duties are equally divided and non attending days we overlap on few days and work independently. We work in wider MDT so all complex patients are known to the whole team but there is a lead consultant for them. Communication is most vital in parttime working and we have a group email, whatsapp group for urgent work and we also have rota so ward team know who is available from our speciality
"There are several advantages and few disadvantages of working part time:
- I enjoy flexibility of working and gives me breathing time in a very busy DGH setting
- It is good for work life balance
- Our trusts supports and have encouraged it
- Communication is most imp key for successful working
But there are some limitations:
- Sometime you land up doing a full time job in a part time contract
- Need to spend little extra time for communication between us and wider team
- Occasionally miss out on teaching or governance meetings which are happening on the day off
Dr Anita Modi, Consultant Paediatrician







