What is an expert witness?
Expert witnesses play an extremely important role in the administration of justice. The Academy of Medical Royal Colleges has set out clear standards for healthcare professionals undertaking expert witness work in terms of report writing, their duty to the court, and their responsibility. An expert witness will:
…assist the court on matters which are outside the knowledge and experience of the court and which, by virtue of their knowledge, training, or experience, are within the healthcare professional’s field of expertise. An expert witness will not, other than in highly exceptional circumstances, have been personally involved with the patient in the case and must declare any potential conflicts of interest.
Normally the expert will be asked by solicitors or other parties if they are willing to accept instruction to assist in the case by providing an expert report.
Healthcare professionals may act as expert witnesses in the following settings:
- coroner's court - to assist the coroner in determining the fact and circumstances of the death
- criminal court
- family court - the RCPCH and the Family Justice Council have produced specific guidance
- civil court - to settle claims of clinical negligence or personal injury brought by patients
- tribunals/fitness to practice settings held by professional regulatory bodies (e.g. GMC) or public enquiries.
Similar standards are expected of healthcare professionals appearing in all these settings, in terms of being aware of the relevant procedure, the purpose of the report and acting with professional competence and integrity.
Healthcare professionals asked to be an expert witness will usually have been required to provide an expert opinion first to help the relevant organisation (police/Crown Prosecution Service, regulatory bodies, medical defence organisations, and solicitors in civil/legal cases) determine whether to take a case to court.
Challenges common to both the external second opinion (ESO) and expert witness processes
Nationally, there is a shortage of paediatricians willing to undertake expert witness (EW) work in relation to family court proceedings. In some specialities, such as paediatric critical care, there is a limited pool of consultants prepared to undertake both types of work. There is obvious overlap between healthcare professionals who choose to do expert witness or medico-legal work, and ESOs.
Both ESOs and expert witness work are on a continuum in that they may relate to the same patient, involve the same group of experts and demand very similar expectations in terms of integrity and governance. The relative shortage of experts is problematic since it frustrates both judicial process and good medical care.
There are several reasons are for this shortage:
- perceived criticism by lawyers, the press, and the judiciary (EW)
- unwarranted social media attention (EW)
- that the work is hugely time consuming and yet relatively poorly remunerated (EW and ESO)
- court processes (e.g. inflexibility of timetable) (EW)
- lack of support (by NHS Trusts) and training (EW and ESO).
The President of the Family Division Working Group on Medical Experts in the Family Courts has made recommendations to address the shortfall of experts prepared to undertake EW work. Justice Williams suggests that solutions will require “engagement at senior level with Department of Health and Ministry of Justice as well as the NHS”. It is suggested that many of the proposed solutions may also address the shortfall of healthcare professionals prepared to undertake ESO work to the extent that both processes will jointly benefit; namely:
- action by the Royal Colleges/professional bodies to create online resources to support EW work and to increase awareness of training in the field provided by organisations such as the Academy of Experts and the Expert Witness Institute
- encouragement to the Royal Colleges/professional bodies to engage with commissioners and/or Trusts to promote a more supportive environment to medical professionals/allied health professionals who wish to undertake EW work
- that the Royal Colleges/professional bodies and the Family Court engage with NHS England and clinical commissioning groups to seek changes to contracting arrangements to enable healthcare professionals to undertake EW work within the parameters of their employment contracts
- creation of greater training opportunities for medical professionals/allied health professionals, including mini-pupillages with judges, cross-disciplinary training courses with medical and legal professionals, and mentoring, peer review and feedback opportunities.
Relationship and differences between ESO and EW work
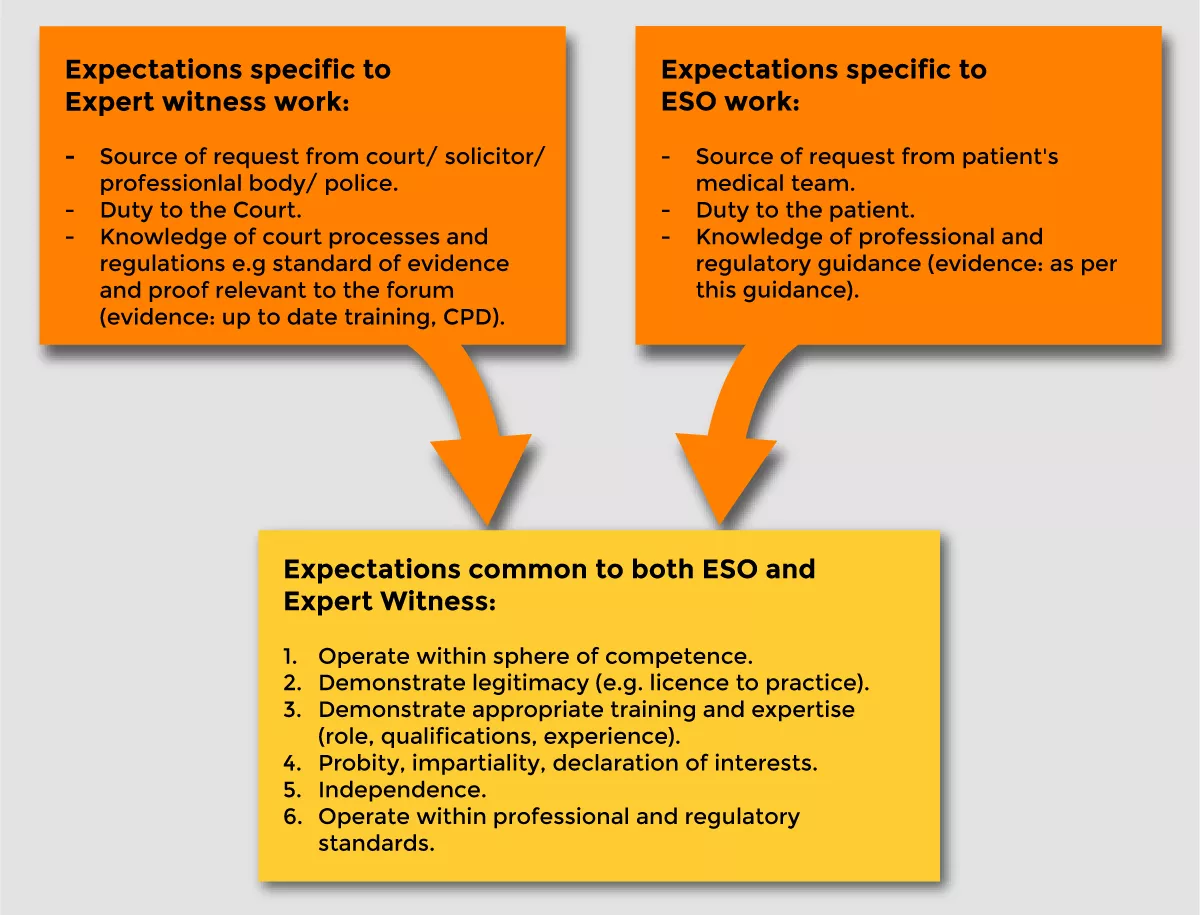
Figure 1 illustrates the relationship between ESO and expert witness work.
Key terms and definitions
- List of key terms and definitions
-
Child or children Babies, children and young people under the age of 18 across the UK. Critical friend A trusted professional, usually within the same organisation, who is requested to offer a critique of a colleague’s management of a challenging situation; for example, either to advise on treatment decisions or to help navigate circumstances where the child’s family and clinical team disagree on the correct course of action. Clinical Ethics Advisory Committee (CEAC) A group consisting of health and other relevant professionals who provide advice and support to clinicians and families on ethical issues that have arisen during clinical practice. Expert witness A healthcare professional, generally appointed by a solicitor, whose skills and experience qualify them to testify on a particular medical area in a court or tribunal setting. External second opinion (ESO) An external medical opinion on the patient’s proposed course of treatment from a second independent health professional/MDT within an appropriate specialty. The initial suggestion to get an ESO may come from a patient/family, or from the child’s health care team. This is for children facing significant life changing decisions, and the second opinion should come from a separate Trust or Health Board. Family Parent, carer or guardian identified as the person with parental responsibility of the child. This could include the local authority. Family advocate A named point of contact who can provide information to and from the family on the ESO process, and who can signpost to sources of support. See this section for more information. Health organisations NHS Trusts and NHS Health Boards across the UK. Healthcare professional A clinically qualified person who is working within the scope of practice as determined by their relevant professional body and who is registered with that body as competent to practice. Mediation An impartial service designed to support patients, families and NHS staff work together towards resolution of disagreements. Multidisciplinary team (MDT) A group of professionals from one or more clinical disciplines from hospital and community settings who together make decisions regarding recommended treatment of individual patients. Named consultant A named consultant taking on overall clinical responsibility for the child. National Advisory Panel A multidisciplinary team of experts organised at national level to support decision making around treatment options in complex and rare diseases. Such panels may enhance consistency and transparency around care pathways and aim to ultimately improve survival outcomes. Parallel planning Parallel planning offers an opportunity for children with life limiting conditions to live their lives to the full while plans are made for managing their ongoing care and end of life. Referral for second opinion The administration and paperwork that is required to support the process of requesting an external second opinion. Service planner Organisations responsible for planning, commissioning, or providing health services. Team around the child The professionals that contribute to the wider health and wellbeing of the child. This would include the child’s named consultant, the MDT, GP and any professional in an advocate role.









