
This blog was produced for the RCPCH Safety eBulletin (April 2025), found here.
The 2025 RCPCH Annual Conference in Glasgow was the largest meeting of child health professionals in the UK this year, attracting 2,900 delegates from across the world. It provided a unique forum for networking, professional development, and the sharing of innovation to improve clinical practice and patient outcomes. This year’s conference stood out for us as it featured many dedicated sessions on patient safety, quality improvement (QI) and culture change. The message was clear: patient safety in paediatrics must remain at the heart of everything we do.
Culture eats strategy for breakfast
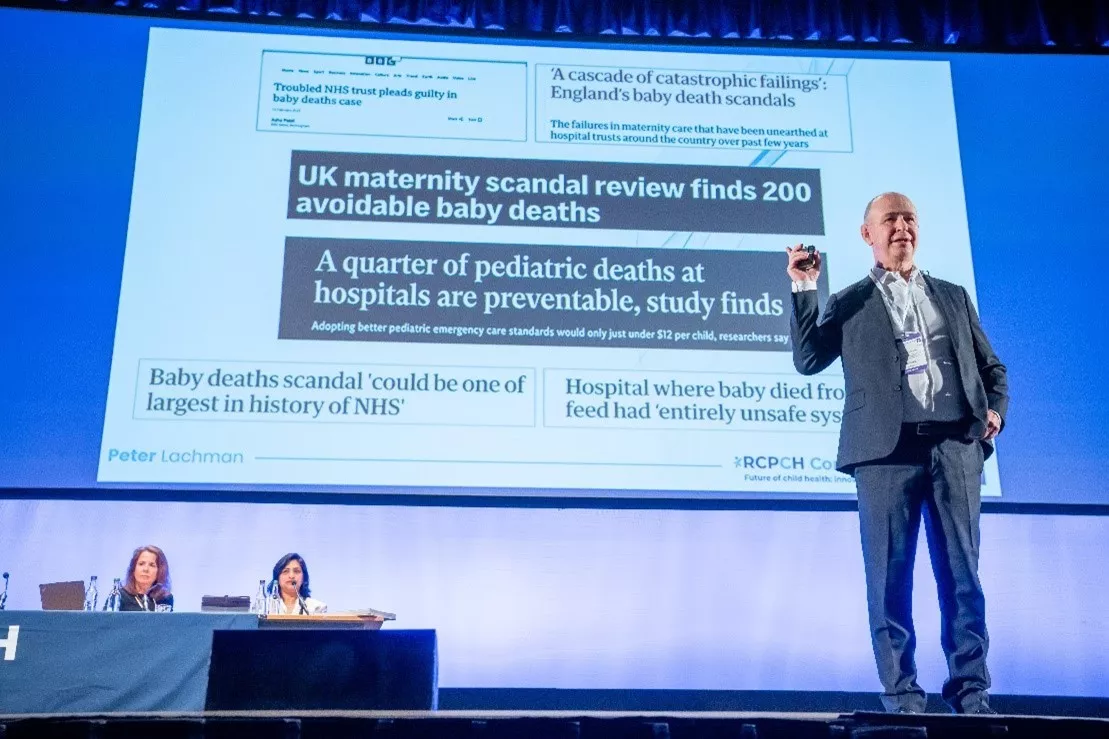
The morning plenary on day 2 of the conference featured a keynote by paediatrician Dr Peter Lachman on "Inspiring a Culture of Safety". Renowned for his expertise in patient safety and Lead Faculty Quality Improvement at the Royal College of Physicians of Ireland, Dr Lachman articulated a compelling vision for a paediatric service where every member of staff is invested in safe care. From his experience of the SAFE (Situation Awareness for Everyone) programme, he argued that patient safety is a shared responsibility across all levels of the organisation, and that effective leadership is essential to cultivate an environment where safety is not merely an aspiration, but a daily practice.
"Culture eats strategy for breakfast", he said. No matter how robust a safety strategy might be, its success is inherently dependent on a culture that prioritises openness, learning and continuous improvement.
Peter invited paediatricians to take the lead in transforming their environments, advocating for visible leadership, active mentoring and a commitment to cultivating psychological safety within teams. His message resonated with many in the audience, serving as a powerful call-to-action for clinicians to re-examine and reinforce the safety frameworks within their own departments.
Sustainable change from the next generation of clinicians
The Quality Improvement and Patient Safety session began with an insightful overview by Jonthan Bamber, Head of Quality and Safety. He presented the RCPCH QI strategy, highlighting the College’s commitment to embedding QI into everyday practice, and our newly launched QI Community.
Next was a series of abstract presentations - mainly from resident (trainee) paediatricians – who shared excellent projects on topics including criteria-led discharges and national safety standards for invasive procedures. The next generation of clinicians recognise that real, sustainable change begins at the grassroots level.
The session included a particularly impactful talk by Dr Sonja Joseph and Tim Sherman from Healthcare Improvement Scotland on the Scottish Patient Safety Programme (SPSP). Dr Joseph addressed the practical challenges and successes of implementing patient safety interventions across complex healthcare systems. Both speakers offered practical insights on how to overcome barriers, engage multidisciplinary teams and foster a culture where every member of the organisation is accountable for safety. They signposted valuable resources, including an online resource hub to support local improvement efforts.
On Ryan’s Rule, clinical guidelines and invited reviews
One of the plenary speakers on the main stage was Professor Nitin Kapur who shared how Australia’s Ryan’s Rule – similar to Martha’s Rule now being piloted in England – has been implemented over the past decade. (Update, 28 May - Professor Kapur wrote about the lessons from Ryan's Rule for our Safety eBulletin for members, published on this website).
At the guideline session, Dr Jan Dudley (RCPCH Registrar) and Dr Sue Protheroe (Officer for Clinical Standards and QI) provided an overview of the RCPCH guideline strategy as well as a resource hub to support specialty groups with guideline development.
A session on improvement and patient safety reviews saw rich discussions on the College’s invited reviews service, how we can support colleagues and departments, and challenges associated with translating recommendations into action.
After the morning plenary on each of the three days, top scoring abstracts are presented. And several were on QI. These included showing safety videos in paediatric emergency departments and bringing empathy and family voices into the most difficult conversations during childhood death review process.
A relentless commitment to safety and QI
Reflecting on our time at Conference, we identified a few key themes:
- Transformative safety improvements begin with leadership that fosters a supportive, learning-oriented culture.
- Empowerment at every level is important.
- The involvement of patients’ families improves outcomes.
- Sharing experiences and resources helps build a robust, resilient and collaborative community.
So this year’s event served as a powerful reminder that excellence in paediatric care is achieved through a relentless commitment to safety and QI. The networking, the innovations and the shared experiences continue to set new benchmarks that we can all take back to our workplaces to improve patient care.
It is only through collective effort, leadership and the unwavering dedication of every team member that we can transform our current practices into a future where patient safety is not just an ideal, but a consistently realised reality.







