These recommendations use the most up to date evidence to inform practice that will enable recovery of children’s elective surgery.
To get an email notification of each update, you can log in and select the pink button in the grey box 'Notify me when updated'.
If you have any questions relating to this guidance, please contact us on health.policy@rcpch.ac.uk.
Background
There has been a significant shift in NHS England and UK government policy following the rollout of vaccines and development of effective antiviral medications; the focus is now on living with respiratory viruses instead of specifically focusing on SARS-CoV-2. In addition, there is now a focus on addressing the huge backlog of procedures which have been delayed since the beginning of the pandemic in a safe and effective way.
Aim
These recommendations use the most up to date evidence to inform practice that will enable optimisation of children’s elective surgery in order to safely address this backlog, whilst maintaining processes to minimise nosocomial spread of SARS-CoV-2. Unnecessary delays pose a very real harm to children if their surgery is delayed any longer than necessary. Due to the significant shift in approach towards SARS-CoV-2, along with the significant experience of NHS staff in standard infection control and prevention processes, these guidelines have been vastly condensed compared to previous versions, allowing a focus on the key changes in guidance.
You can download the November 2021 version of the guidance below.
We will continue to be vigilant and will update this guidance should community prevalence of COVID-19 change in the future.
Scope
The June 2022 guidance update has been developed by representatives from NHS England/Improvement, Royal College of Paediatrics and Child Health, the Children’s Surgical Forum, British Association of Paediatric Surgeons, and Association of Paediatric Anaesthetists of Great Britain and Ireland.
The June 2022 guidance update is endorsed by Royal College of Paediatrics and Child Health, British Association of Paediatric Surgeons, Association of Paediatric Anaesthetists of Great Britain and Ireland, and Royal College of Anaesthetists.

It builds on 2020/2021 guidance developed by NHS England/Improvement, UK Health Security Agency, the Royal College of Surgeons of England, Royal College of Anaesthetists, Royal College of Paediatrics and Child Health, the Children’s Surgical Forum, British Association of Paediatric Surgeons, Association of Paediatric Anaesthetists of Great Britain and Ireland, and The Association for Perioperative Practice. You can download the November 2021 version of the guidance below.
While some recommendations focus on the systems organised in England, services in the devolved nations are encouraged to adopt them to fit local models.
Updates
Updates in this version (June 2022):
- Pre-op SARS-CoV-2 testing is not required prior to elective surgery in children, irrespective of vaccination status and irrespective of whether the child requires an overnight admission. Only if a symptomatic child undergoing elective surgery is being admitted to a critical care unit or is likely to be in close contact with extremely vulnerable* children post-op should multiplex PCR testing for a panel of respiratory viruses be considered, in order to inform infection prevention and control practices.
- All children undergoing elective surgery should have symptom-based pre-op screening performed in the 72 hours prior to surgery; if this identifies symptoms consistent with a respiratory tract infection, a decision needs to be made by the anaesthetist about the safety of anaesthetising the child for surgery.
- Elective surgery does not need to be deferred in children following asymptomatic or mild COVID-19 infection. However, in hospitals still requiring isolation of patients following infection with SARS-CoV-2, it is reasonable for elective surgery to be delayed for this period to reduce pressure on isolation facilities.
* those with severe underlying respiratory disease, congenital heart disease with persisting heart failure or cyanosis or severe immunodeficiency
Rationale for changes to guidance in June 2022:
- The vast majority of children have been infected with SARS-CoV-2 at some point during the pandemic:
Table 1. Proportion of age band with previous SARS-CoV-2 infection (UKHSA data)
| Age | Proportion with previous SARS-CoV-2 infection |
|---|---|
| <1yr | 75.4%(74.6%-76.1%) |
| 1-4 | 87.1%(86.6%-87.7%) |
| 5-14 | 96.8%(96.5%-97.1%) |
| 15-24 | 92.5%(92.1%-92.9%) |
| 25-44 | 82.9%(82.5%-83.4%) |
| 45-64 | 71.9%(71.4%-72.4%) |
| 65-74 | 59%(58.5%-59.6%) |
| 75+ | 59.7%(59.1%-60.3%) |
- Natural infection is likely to provide similar protection to vaccination; mandating full vaccination status to avoid pre-op testing in asymptomatic patients is hard to justify, especially as children under 12 years of age have only been offered the vaccine since April 2022 and children under 5 years of age are not being offered the vaccine. This approach is discriminatory and is most likely to adversely impact the most vulnerable children/families who will find performing pre-op testing most challenging.
- Using pre-op testing to reduce transmission of COVID in hospital should not be an ambition in children as they are unlikely to get unwell if infected with COVID, they are unlikely to expose vulnerable adults in hospital, the majority of staff and vulnerable adults/children have been fully vaccinated against SARS-CoV-2 and there is no evidence to suggest increased post-op mortality or mobility in children. National COVID strategy has moved away from trying to avoid transmission in society as of 24 February 2022.
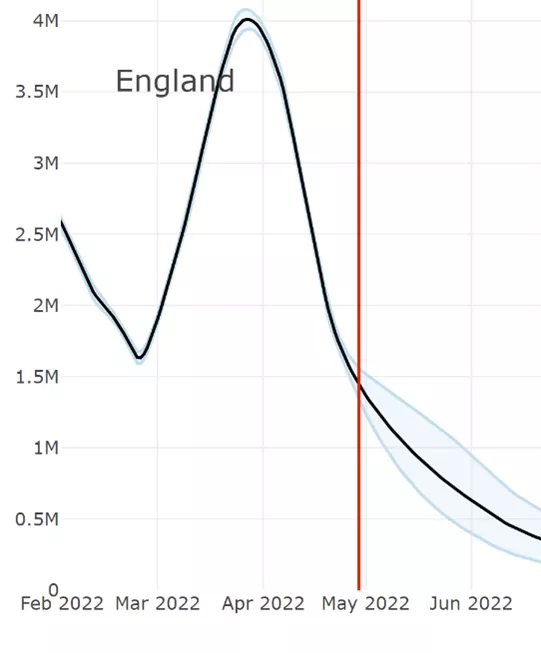
- Rates of SARS-CoV-2 have reduced markedly the UK, with prevalence <1% by end of May 2022 (UKHSA data):
Summary of recommendations
- Prioritisation of surgical cases should be undertaken according to clinical urgency as per the Federation of Specialty Surgical Associations (FSSA) Clinical Guide to Surgical Prioritisation During the Coronavirus Pandemic.
- Theatre scheduling should ensure that every list is used effectively and efficiently.
- Pre-operative SARS-CoV-2 testing is not required prior to elective surgery in children, irrespective of vaccination status and irrespective of whether the child requires an overnight admission. Carers or parents accompanying the child to hospital for the procedure do not require routine swabbing.
- Elective surgery does not need to be deferred in children following asymptomatic or mild COVID-19 infection. However, in hospitals still requiring isolation of patients following infection with SARS-CoV-2, it is reasonable for elective surgery to be delayed for this period to reduce pressure on isolation facilities. In children with severe symptoms associated with COVID-19 infection, an anaesthetic review is required to decide the duration of delay. Repeat SARS-CoV-2 testing is not recommended prior to elective surgery. Exemption - Immunocompromised children: in these children a clinical risk assessment should be carried out in conjunction with the IPC team and virologists.
- All children undergoing elective surgery should have symptom-based pre-op screening performed in the 72 hours prior to surgery; if this identifies symptoms consistent with a respiratory tract infection, a decision needs to be made by the anaesthetist about the safety of anaesthetising the child for surgery. Only if a symptomatic child undergoing elective surgery is being admitted to a critical care unit or is likely to be in close contact with extremely vulnerable** children post-op, should multiplex PCR testing for a panel of respiratory viruses be considered, in order to inform infection prevention and control (IPC) practices. Pre-operative isolation is not recommended as a routine practice for children undergoing elective surgery.
- Children and their parents/carers should have the opportunity to discuss the procedure prior to elective admission and have access to written information. During the discussion, it should be explained that there is a small chance of the child and/or parent/carer acquiring COVID-19 in hospital. Whenever possible, consent will be taken prior to admission.
- Acute Trusts should ensure that IPC measures put in place during elective surgery align with guidance within the National IPC Manual (PDF).
- Consistent messaging regarding hand hygiene and face coverings should be maintained throughout the hospital to reinforce that these infection prevention and control measures are the most effective way of reducing the transmission of infections. See also the National Standards of Healthcare Cleanliness 2021.
- Normal post-operative observations and care pathways should be followed.
- Rapid discharge after day case procedures should be supported and encouraged.
- Provider / Regional / National monitoring of elective surgery activity including the rates of cancellations should be undertaken.
** those with severe underlying respiratory disease, congenital heart disease with persisting heart failure or cyanosis or severe immunodeficiency
How long should elective surgery in children be delayed following COVID-19 infection?
There is currently wide variation in practice between hospitals in how long elective surgery is delayed following a diagnosis of SARS-CoV-2 in a child. In some centres, elective surgery in children is being routinely delayed by 7 weeks following infection with SARS-CoV-2.
Although it is reasonable from an anaesthetic perspective to delay elective surgery for several weeks after a severe case of respiratory COVID (requiring admission to hospital) and there is a rationale for delaying elective surgery in children who experience chronic symptoms (long-COVID) following SARS-CoV-2, both of these scenarios are fortunately relatively rare in children. The vast majority of children with SARS-CoV-2 have mild or asymptomatic disease and, in this situation, the rationale for delaying elective surgery should be considered in terms of the following:
- IPC – concerns over transmission to other children and clinical staff:
- There is a large body of evidence showing that the risk of onward transmission of the currently circulating SARS-CoV-2 strains is extremely low beyond 10 days from onset of symptoms / diagnosis in immunocompetent children.
- However, many hospitals require isolation of patients for the 10 days following the onset of symptoms / diagnosis. For this reason, the steering group feel that in acute trusts that require isolation for 10 days following the onset of symptoms/diagnosis of SARS-CoV-2, it is reasonable for elective surgery to be delayed for this period to reduce pressure on isolation facilities.
- The steering group do not feel that repeat SARS-CoV-2 testing is necessarily required prior to elective surgery. However, if repeat testing is performed, systems should be in place to measure the PCR cycle threshold (CT) value – a positive PCR test with a CT value of over 35 suggests an extremely low likelihood of viable virus and thus almost no ongoing transmission risk when standard infection control processes are in place. Another option would be to use a lateral flow test in this situation.
- For immunocompromised children, a clinical risk assessment needs to be performed to determine how long surgery should be delayed. This should be done in conjunction with the infection control team and clinical virologists.
- Risk from SARS-CoV-2 as a co-morbidity to the underlying illness / intervention:
- Peri‐operative outcomes of children with SARS‐CoV‐2 infection are favourable compared to adults1
- Based on the evidence and expert consensus it was agreed by the steering group that the approach to SARS-CoV-2 and elective surgery in children should be different to adults, resulting in a shorter delay to elective surgery. Data will be continued to be collected on the outcomes of children requiring emergency surgery shortly after a SARS-CoV-2 infection and this guidance will be reviewed accordingly.
- 1Nepogodiev D. Favourable perioperative outcomes for children with SARS‐CoV‐2. British Journal of Surgery 2020; 107: e644–e645










