As you may know, the College is in the process of redesigning paediatric training.
We have completed the first phase - the implementation of the Progress curriculum. And now we are focusing on the shape of the training pathway, namely how long, which posts, in what order, etc.
There is more information about our plan on the RCPCH website, but for this blog I thought I would share some of thoughts and ideas we have debated along the way.
We need a more flexible pathway
Allowing trainees and programme directors more flexibility is really about enabling choice: inflexible pathways restrict choice.
I was pleased to see that the need for doctors to have some autonomy and control over their working lives has been recognised as the “A” in the “ABC” of core needs in the recent report, Caring for doctors, caring for patients, by Professor Michael West and Dame Denise Coia.
While we can’t offer completely free choice, I certainly believe that trainees should have more options available to them during training. Children and families benefit from being treated by a workforce with a more varied experiential base and a more diverse skill set.
How will the new training pathway be more flexible?
The first four years of the pathway will not be defined by placements, but by what needs to be achieved in terms of learning outcomes. This will give programme directors more flexibility in how they use new and existing placements to construct programmes.
A two-level model (core and specialty paediatrics) imposes less restriction upon progression than the current three-level pathway. Trainees should be able to move to the specialty level when they are ready, able and have completed MRCPCH. And there will no longer be an imposed time-based requirement to undertake all the components of the current level 2 (general paediatrics, community child health, neonatal medicine).
We are looking at ways trainees might be able to move from one sub-specialty pathway to another if they realise that an alternative pathway is more suitable. Many of our current sub-specialty syllabi share content, and therefore it should be possible to transfer without necessarily prolonging training time. This this would depend on the nature of the origin and destination sub-specialties and we'd also need to ensure any transfer process is both feasible and equitable.
Out of programme (OOP) and less than full time (LTFT) opportunities
Health Education England has extended the LTFT pilot to paediatrics, which is great news. Now trainees can apply to work less than full time without needing to fulfil category 1 or 2 criteria. I do hope most, if not all trainees, who apply are given this opportunity.
A more fluid and less predictable workforce is... preferable to one in which there is high attrition...
There is also increasing recognition that we must allow trainees more freedom to take OOP opportunities. Having an outcomes and capability-based curriculum means that capabilities gained during OOP are not “lost” or “ignored”, as may be the case with time-based training. Trainees returning from OOP, who are now more capable than when they left, should be able to progress through their subsequent training faster.
The workforce might be destabilised if we grant more autonomy to trainees in determining how they train. We need to take that risk. A more fluid and less predictable workforce is still more preferable to one in which there is high attrition and potentially fewer people left to do the work.
Length of training
About 52% of people tell me the current training is too short and 48% say it is too long – or is it the other way round? Is there a Goldilocks length or is the perception of training time subject to wide individual variation?
Some foundation year doctors may be put off by the thought of eight years of training and some trainees can feel little sense of progress, despite having started training many years ago. However, there is the concern that shortening training will produce poorly skilled and inexperienced consultants.
Training pathways aim to produce consultants who are “good enough” for the service needs of the time. Different jobs will require different skills, and thus the solution is that the pathway cover core essentials but allow trainees to supplement training through OOP experiences, to meet the varying demands and expectation of employers.
Run-through training
Didn’t all our problems with rota gaps start when we moved to a run through programme? Possibly - but association doesn’t prove causation. Times have changed. I don’t believe we should force every trainee to re-apply for their job, particularly when there is no current competition! However, I do believe we should allow them to take OOP between levels, if that is what they want.
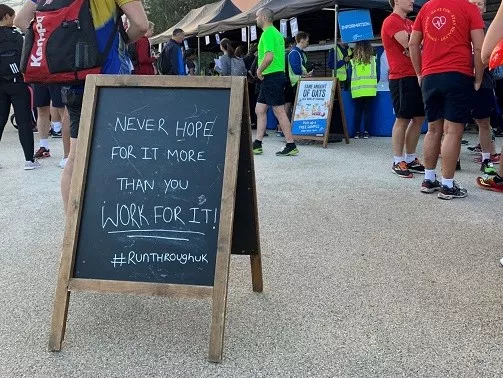
Now for the tenuous link to this month’s photographs. If, like me, you find yourself staying over in London on an occasional Wednesday evening, I can recommend one of the regular 10k evening runs organised by RunThrough – very friendly, marshalled course, chip timings and flapjack! Last week, I was thinking of what to write in this blog as I plodded around the four-lap course. As the rain started to descend, I suddenly saw an advantage to being able either to take time out of programme or to go for an early finish...