Background
Research has shown that magnesium sulphate (MgSO4), given antenatally in threatened preterm labour, is neuroprotective and reduces cerebral palsy. Watford General Hospital was an outlier for this audit measure in the 2017 NNAP report (2016 data).
In this case study, we demonstrate how we have used NNAP antenatal MgSO4 data to guide our quality improvement in MgSO4 uptake.
Our improvement journey started in 2016, when we became aware that our neonatal service was an outlier for antenatal magnesium sulphate (MgSO4) administration with an uptake of about 20%, which was far below the national average (43%).
What we did
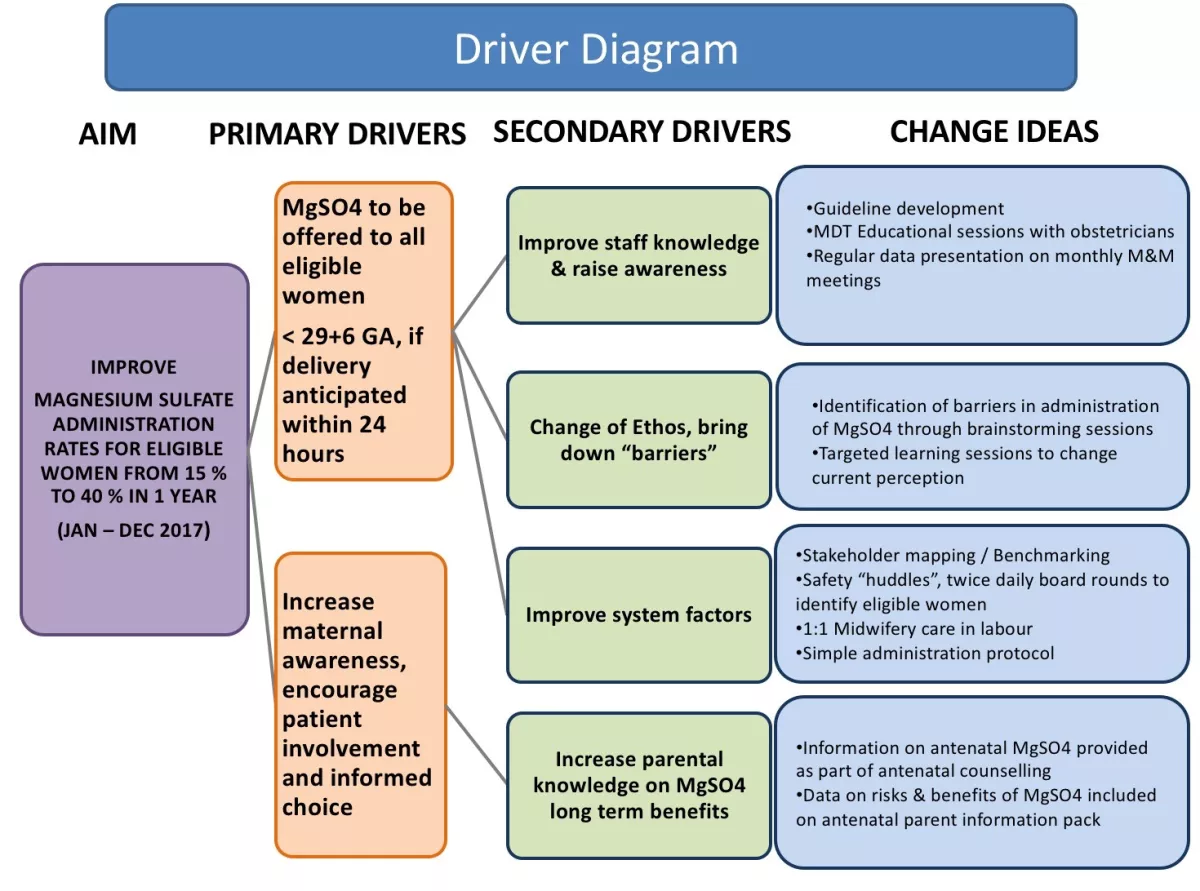
Using the Institute of Healthcare Improvement (IHI) model we aimed to increase the uptake of MgSO4 in eligible preterm deliveries. Improvement was defined as an increase in the uptake of MgSO4 from 15% in 2016 to 40%, hence reaching the then national average.
Primary and secondary drivers were identified which informed change ideas (as shown in Figure 1 below). These changes were tested in iterative plan, do, study, act (PDSA) cycles.
Change package
We increased awareness among the neonatal, obstetric and midwifery teams by presenting run chart data (Figure 2) in monthly perinatal mortality and morbidity meetings.
We commenced frequent bitesize MgSO4 awareness and engagement sessions with all the stakeholders.
A new and simple guideline for MgSO4 administration was developed and implemented, and we encouraged 1:1 midwifery care in labour. Safety “huddles”, twice daily board rounds, were introduced to identify all eligible women.
Additionally, we involved the service users, by providing them with a parental information leaflet with the antenatal counselling pack. MgSO4 information was included in the antenatal counselling conversations and golden hour care checklist.
Challenges
The main challenge was to change staff’s ethos and perceptions, bring down the “barriers” and move away from the culture, “this is how we do it for years and it works for our patients”. We achieved this by enhancing communication and knowledge sharing through safety huddles, identifying clinical champions to support the team, presentations in joint multidisciplinary team forums and empowering ward level leadership.
Encouraging parent involvement raised further awareness of this important neuroprotective treatment.
What we achieved
According to the NNAP 2016 report only 15% of eligible women received antenatal MgSO4 at Watford General Hospital, compared to a national average of 43%. Table 1 and Figure 2 shows steady improvement from 2016 to 2018 with the implementation of change ideas. The 2017 data show that we met and surpassed our improvement target achieving a compliance of 55%, well above the national average. The 2018 NNAP data shows further improvement and a sustainable change. This sustainable improvement has a direct impact on the long-term neurodevelopmental outcomes and by extension to the quality of life of preterm babies born at less than 30 weeks of gestation.
| Year | Eligible mothers | MgSO4 | MgSO4 not given |
|---|---|---|---|
| 2016 | 20 | 3 (15%) | 17 (85%) |
| 2017 | 18 | 10 (55%) | 8 (44%) |
| Jan-May 2018 | 6 | 5 (83%) | 1 (17%) |
Top tips for implementation
- Identify an appropriate maternity-neonatal forum to share NNAP MgSO4 data.
- Identify and engage stakeholders and frontline champions within maternity and neonates.
- Use live NNAP dashboard on BadgerNet to generate live run charts.
- Partner with parents for improvement.
Presented by
Dr Sankara Narayanan (Consultant Neonatologist & NNAP lead), Dr Anastasia Katana (Locum Consultant Neonatologist), Ms Nanda Shetty (Consultant Obstetrician), Ms Marcellina Coker (Consultant Obstetrician)
Neonatal & Obstetrics Department, Watford General Hospital, West Hertfordshire NHS Trust
Acknowledgements
Justine Chung, Matron, Delivery Suite, Bhavani Sivakumar, BadgerNet Data Analyst