What was the challenge?
Sheffield Children’s Hospital is one of a few dedicated children's hospital trusts in the UK and a paediatric major trauma centre, providing paediatric services to children across South Yorkshire.
Over the last five years, there has been a 2.3% average yearly increase in attendances to the Emergency Department (ED). In addition, despite investment in medical and nursing staff levels, it faces the same medical staff shortages on junior doctor rotas that are reflected across country. In a 12 month period, 12.7% of our attendances meet primary care triage criteria; this rises to 15.2% in winter months.
What did you do?
In response to the rising patient demand and the medical staffing challenges, a GP streaming model was introduced:
- Patient registers at ED reception
- Patient sees triage nurse who decides if appropriate for primary care
- Patient sent to separate waiting area for GP
- Patient seen and then discharged by GP. Any follow up with home GP
Triage
Each patient is assessed by a triage nurse, including a full set of observations. If they meet the primary care triage criteria (Figure 1), they can be streamed to the GP service during its hours of operation.
At triage, POPS (Paediatric Observation Priority Score) is used when assessing observations1. The ED nurse coordinator is responsible for overseeing patient flow.
|
Well children over 3 months old POPS score 0-2 with NO red features No chronic medical problems
|
The GP service
The service employs one GP who is co-located on a corridor between the ED and paediatric assessment unit. The room is separate to the ED but located close by, which ensures help and advice are available. The ED consultant is available for support and discussion of clinical cases if required. The GP has 20 minute appointments.
The GP is supported by a healthcare assistant who provides clerical support, carries out patient observations and urinalysis.
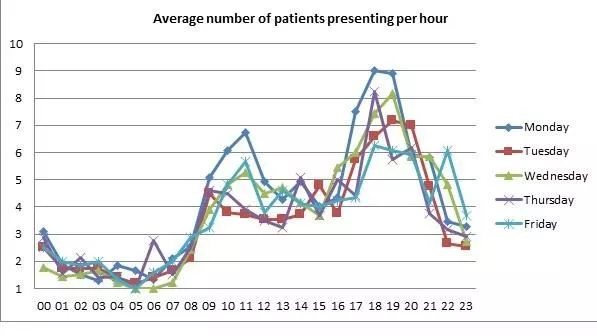
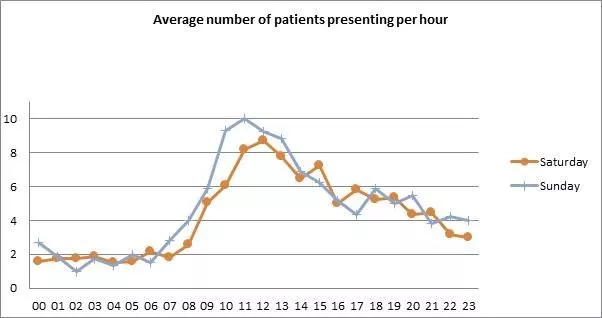
The GP service operates Monday to Friday, 18:00 - 23:00, and Saturday to Sunday, 11:00 - 20:00 during school terms. This was based on analysis that considered patient demand, ED activity levels and primary care provision elsewhere in the city.
The GP has access to the same pathways for referral and investigations as they would do working in other GP out-of-hours services in the city. They also use the primary care electronic medical record system.
When the GP has more than six patients waiting, or the wait to see the GP is greater than two hours, or when there is no GP on shift, the ED staff will see patients in the primary care triage category.
What was the impact?
Sheffield Children’s Hospital was already a top performing Trust, meeting the four-hour target 97% of the time. This success has continued since the introduction of primary care streaming despite an increasing number of attendances.
In the first hour that the GP service is operational, there is an average reduction in ED length of stay, for all triage categories, of seven minutes.
Figures 2 and 3 below show the average number of primary care patients attending by hour during the week and at the weekend respectively.
The GP sees, on average, 3-4 patients per hour. Primary care patients who see the GP spend 44 minutes less time in ED than those seen by ED staff.
Importantly, there is no significant difference in admission rates when comparing those patients seen by a GP with those seen by ED staff. In addition, the re-attendance rate at ED within seven days is lower for patients seen by the GP (GP 8.5% vs ED 9.1%). Overall ED re-attendance rate, for all triage categories, was 8.6%.
What did it cost to set up?
The project to provide a GP streaming service has involved collaboration between the acute hospital trust, the primary care out-of-hours provider and the clinical commissioning group.
During the initial development stages, a project manager led the team. There is an ongoing time commitment from representatives of the acute hospital trust and the primary care out-of-hours provider who sit on a clinical governance group which meets every two months.
Since the service utilises existing facilities within the hospital, there has been no additional cost for provision of accommodation.
The clinical commissioning group has negotiated a reduced tariff for patients who see the GP, and the GP is employed by the primary care out-of-hours provider. The main cost for the acute hospital trust is the employment of a healthcare assistant.
What advice can you share?
The key to our success has been the focus on a collaborative approach at all stages from the initial service development to the shared approach to clinical governance, with clearly defined lines of accountability.
Collaboration between primary and secondary care providers also provides a unique opportunity for shared learning, which has the added benefit of improving the standard of care children receive in both settings.
For more information please contact: mmccarron@doctors.org.uk.
Disclaimer: RCPCH have been notified that the above is a good example in managing winter pressures in emergency departments and will be reviewed on a regular basis. Sharing examples does not equate to formal RCPCH endorsement.
- 1Roland D., Lewis G., Fielding P., Hakim C., Watts A., Davies F. The paediatric observation priority score: a system to aid detection of serious illness and assist in safe discharge. Open Journal of Emergency Medicine. 2016;4(2):38–44. doi: 10.4236/ojem.2016.42006