
Oxygen is vital to life and we should all live in an equal world and have clean air.
Background and policy context
We strongly support national policies and legislation that aim to improve indoor and outdoor air quality. We encourage child health professionals to share information with colleagues and patients, and use their voices to advocate for clean air. We recognise that air pollution is a global issue requiring international cooperation. For this statement our messages and recommendations are specific to the UK.
Read our quick read report here or download from the bottom of this page.
Key facts
It's hard to know what my local air quality is because we assume that we have good air; no-one tells us where is good or bad air and in which areas.
- Air pollution has overtaken high blood pressure and smoking as the leading contributor to global disease.1 Exposure to air pollution is the second leading risk factor for death in children under 5, both globally and in the UK.2
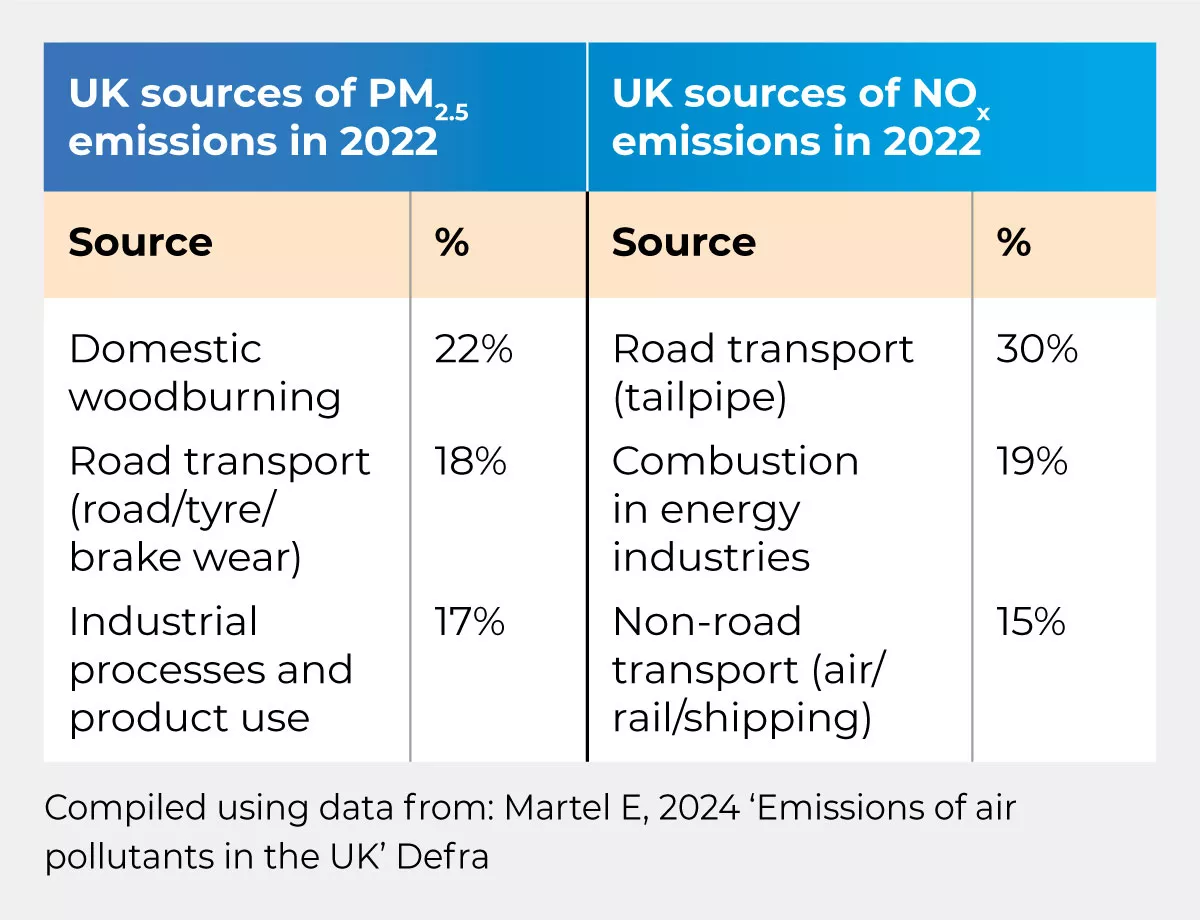
- Fine particulate matter (PM2.5) and nitrogen dioxide (NO2) are responsible for a significant proportion of air pollution’s health impacts.3, 4 The main UK sources of PM2.5 and NOx emissions are highlighted in the table below. (NOx refers to a group of gases that includes NO2).
- Deprived neighbourhoods and minoritised communities tend to experience higher levels of air pollution.5 Individuals living near main roads face higher exposure to vehicle emissions, both outdoors and indoors.6 This particularly affects residents in densely populated urban areas, despite the fact that those living in highly polluted areas are less likely to own a car themselves.7
- The UK government and devolved administrations have not yet committed to meeting the 2021 WHO Air Quality guidelines, which outline air pollution limits designed to protect public health. As demonstrated in the table below, UK targets are currently four times WHO guidance for PM2.5 and NO2, except in Scotland, where the devolved administration has committed to lower PM2.5 targets.
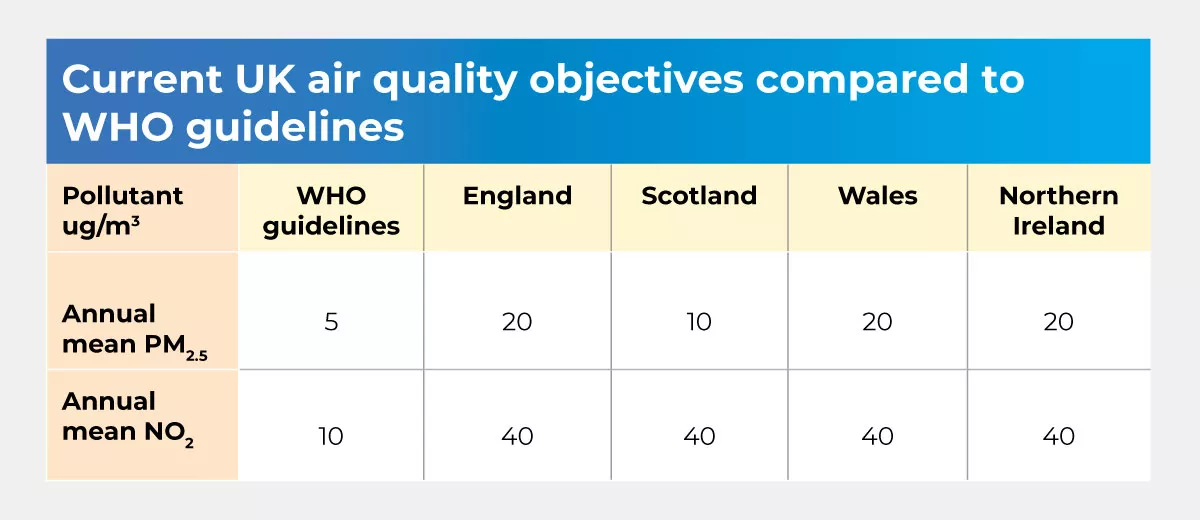
- One in 4 UK residents live in areas with PM2.5 levels more than twice the upper limit of WHO guidelines.8 In 2023, roadside NO2 levels in the UK were over two times WHO guidelines.9 Though WHO guidance sets limits on air pollution, evidence shows that there are no safe limits to exposure, and air pollutants should be reduced as far as possible towards zero.
- Pollutants from outdoors enter buildings and impact indoor air quality. Air quality inside buildings is also influenced by building design, construction materials, furnishings, dust, mould, pets, plants, and activities such as cooking, cleaning, smoking, and woodburning.10 Ensuring there is adequate ventilation to prevent build-up of pollutants is especially important for new building designs and mass retrofitting programmes, which often focus primarily on achieving airtightness for energy efficiency.
- Tobacco smoke has a particularly significant impact on indoor air pollution. Households with resident smokers have been shown to have indoor PM2.5 levels 15-20 times higher than households burning gas, wood, coal or peat.11
- Woodburning releases harmful PM2.5 particles and significantly contributes to indoor and outdoor pollution, and many people are unaware of its health risks.12 Woodburning disproportionately affects vulnerable populations, despite being a prevalent activity in wealthier urban households with access to alternative heat sources.
- Road transport is a significant source of both PM2.5 and NO2. Transitioning to electric vehicles will reduce tailpipe NO2 emissions but PM2.5 emissions from road, tyre and brake wear will continue. Active travel, such as cycling and walking, reduces both PM2.5 and NO2 emissions, and provides additional health benefits from exercise.
- Clean air zones with charging have been modelled by the UK government as the most time-efficient measure to reduce urban NO2 levels to legal limits.13 In Bath, NO2 concentrations have reduced by an average of 25% since the Clean Air Zone was implemented in 2019.14 London’s ULEZ has reduced roadside NO2 levels by 53% in central London, 24% in inner London, and 21% in outer London.15 The Greater London LEZ is estimated to have saved over £0.9 billion in health and labour market costs,16 however there is limited evidence on the socioeconomic impacts of clean air zone implementation on individuals, especially already disadvantaged groups.
- Children spend a significant proportion of their time in school, and governments and local authorities have a duty to protect them during this time. There is inadequate monitoring in and around schools to ensure that children are not put at risk of air pollution exposure during the school day.
Key considerations
I have asthma so it does worry me a lot because pollution plays a big part.
- Air pollution adversely impacts human health throughout the life course. Exposure to air pollution during gestation, infancy, childhood, and adolescence affects developing organs, and increases the risk of chronic disease in adulthood.3, 17
- Children are especially vulnerable to air pollution because they inhale more air than adults in proportion to their body weight, breathe closer to ground-level sources of air pollution such as vehicle exhausts, and are less able to control their exposure than adults.2
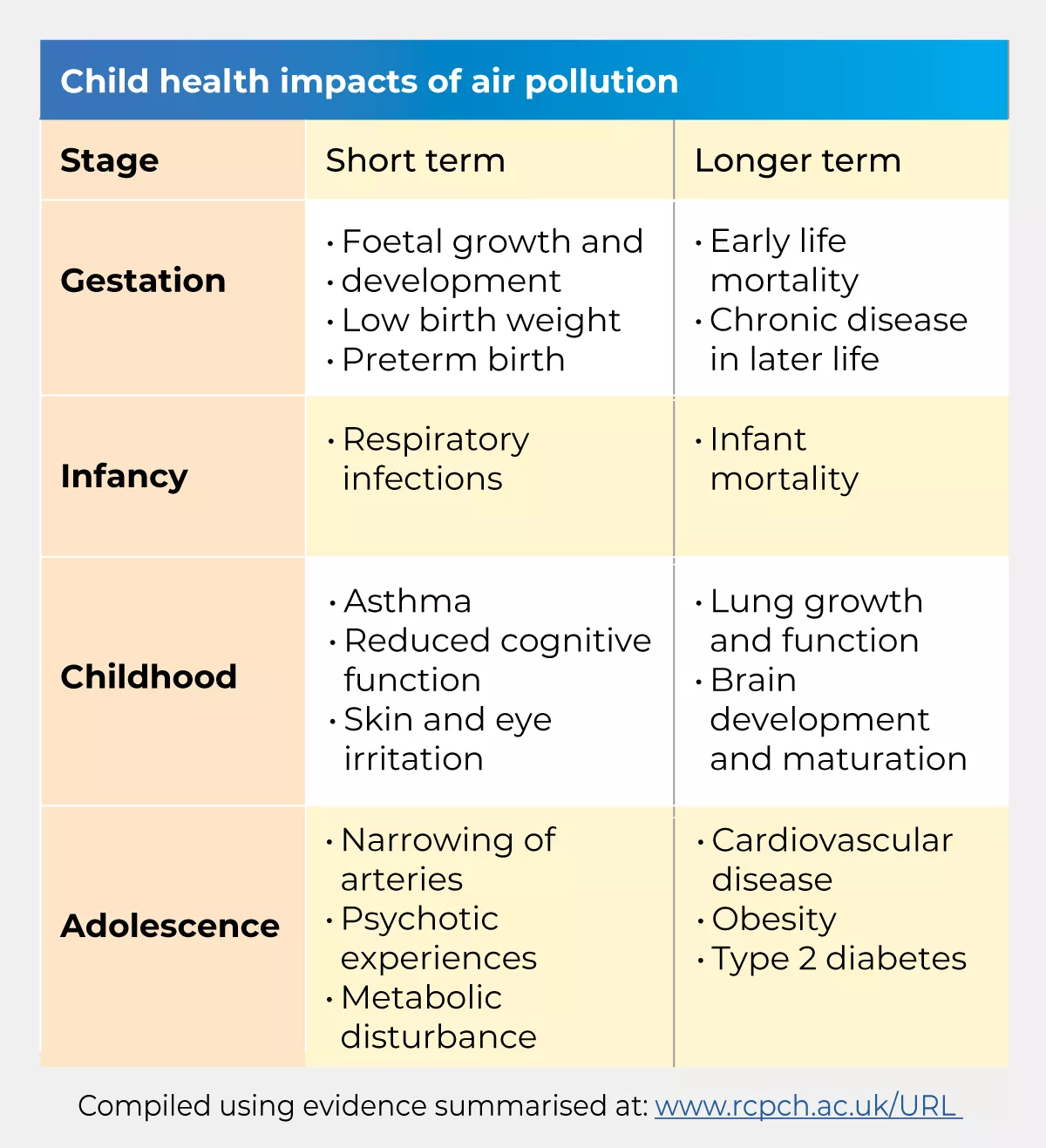
- Asthma: Air pollution increases airway sensitivity and causes lung inflammation. Exposure to air pollution is associated with increased GP respiratory consultations and inhaler prescriptions,18 hospital admissions and deaths. In 2017-19, an estimated 7% of paediatric asthma admissions in London were linked to spikes in air pollution, and reductions in air pollution concentration correlated with reduced hospital admissions.19
- Birth outcomes: Particulate matter inhaled during pregnancy can affect blood flow to the foetus, cross the placenta and reach the foetal bloodstream and organs.20 A significant body of research links maternal PM2.5 exposure to low birth weight and preterm birth, both of which increase the risk of early life mortality and long-term health problems.
- Lung development: Multiple large-scale studies have shown that long-term exposure to air pollution in early life adversely affects lung growth, even at relatively low concentrations. Exposure to air pollution also increases symptom severity and the likelihood of hospitalisation for infant respiratory infections such as bronchiolitis.21 Improvements in air quality have been linked to improved lung function development.22
- Brain development and cognition: Air pollution has been shown to adversely affect brain development and maturation, cognitive function, attention and memory. Exposure of school children to traffic-related air pollution is associated with slowed responses and inattentiveness in computerised cognitive tests.23
- Mental health: Air pollution exposure may also adversely impact mental health and wellbeing. Air pollution has been linked to increased incidence of adolescent psychotic experiences,24 and increased prescriptions for antipsychotic and sedative medications.25
- Cardiovascular health: There is strong evidence of the link between air pollution exposure and cardiovascular disease in adulthood.7 Recent studies show an association between childhood air pollution exposure and atherosclerosis (narrowing of the arteries) in adolescence26 and young adulthood,27 suggesting that early life exposure may increase the risk of cardiovascular disease in later life.
- Metabolic disease: Air pollution has been linked to increased incidence of type 2 diabetes and obesity in adults.28 Research suggests that disease processes may start in childhood.29
- Skin: Air pollution can also be absorbed through the skin and mucous membranes, causing childhood eczema, dermatitis, skin and eye irritation.7
Health inequalities
I’m particularly concerned for marginalised communities who will be most impacted despite not being perpetrators.
Although air pollution affects everyone, structural inequalities mean that some groups are more severely affected. Global inequalities in air pollution’s impact on child health are striking. The air pollution-linked death rate in children under the age of five in East, West, Central and Southern Africa is 100 times higher than their counterparts in high income countries.2
- Exposure: Deprived households are exposed to elevated levels of air pollution. A 2015 study found that the most deprived 20% of neighbourhoods in England had higher air pollution levels than the least deprived, even after adjusting for other factors.30 Causes contributing to this include proximity to busy roads, inadequate construction, insufficient ventilation, and higher occupancy levels. Indoor air pollution exposure is exacerbated in overcrowded homes, where increased movement stirs up dust and particulate matter.
- Adaptation: The impacts of air pollution also vary due to different adaptive capacities available to children, young people, and their families. Low-income households may face inadequate housing options, fuel poverty and limited resources to address damp and mould.
- Vulnerability: Socioeconomically disadvantaged individuals are more likely to have pre-existing medical conditions, increasing their vulnerability to air pollution’s health impacts.
Case studies
- Ella Adoo Kissi-Debrah
-
Ella Adoo Kissi-Debrah, a healthy child, developed severe asthma at 7 years old, which was worsened by breathing polluted air, especially from traffic emissions near her home in Southeast London. This led to her tragic death at age nine. Her death certificate is the first in the world to list air pollution as a cause of death and her case highlights the critical need for stricter air quality measures and better education on the health impacts of air pollution.
- Awaab Ishak
-
Awaab Ishak, a two year-old living in Rochdale, tragically died in December 2020 due to severe respiratory problems caused by exposure to black mould in his home, despite his father repeatedly raising the issue with his housing provider. His death has prompted legal reforms known as "Awaab's Law," requiring timely repairs for damp and mould in social housing. His case underscores the critical need for improved housing conditions and quicker action from housing providers when concerns are raised.
Economic impact
Economic loss: Outdoor air pollution currently costs $2.9 trillion globally31 and 2.6% of the UK's GDP annually.32 These costs are projected to increase to 1% of global GDP by 2060, impacting labour productivity, health expenditures, and crop yields.
Healthcare burden: Air pollution causes a significant burden on our healthcare system. In 2017, the combined NHS and social care costs attributable to PM2.5 and NO2 amounted to £42.88 million. This figure increases to £157 million when considering diseases with less robust evidence of association with air pollution.33
Potential economic gain: Achieving the air quality guidelines set by the World Health Organization (WHO) could bring substantial economic benefits, potentially boosting the UK economy by £1.6 billion annually, according to analysis by CBI Economics.34
Key messages for health professionals
We all breathe so should all care.
Child health professionals can use their trusted voices to influence behaviour, health impacts and policy change through acting at a personal, professional and political level:
Personal: Health professionals are seen as role models within our communities. By educating ourselves and following principles which reduce air pollution emissions and exposure, we can encourage others to follow suit.
Professional: In our clinical practice we need to make air pollution conversation ‘business as usual’. This includes talking to our patients and colleagues about air pollution. We should explain the effects of air pollution on child health, and ways to reduce emissions and mitigate exposure, whilst being mindful not to place blame on individuals. In leadership roles child health professionals should advocate for sustainable clinical practice that reduces air pollution emissions.
Political: Doctors, nurses and pharmacists are consistently among the most trusted professions. We should use this power to advocate for policies that reduce air pollution at local, regional and national levels.
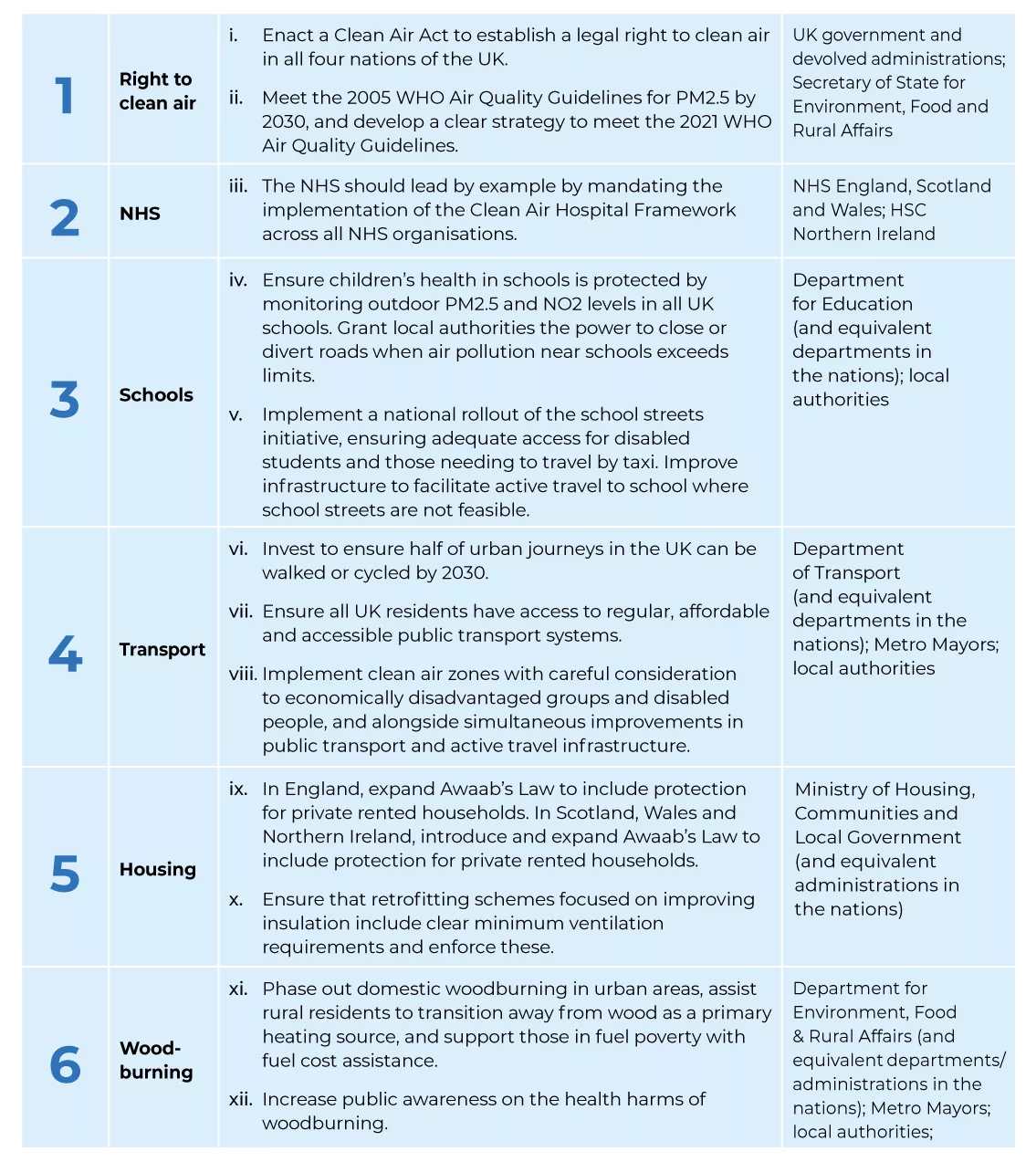
Recommendations
Air pollution is an avoidable cause of morbidity and mortality, and measures to improve air quality often have additional health and environmental co-benefits. Already deprived populations, despite contributing less to air pollution, experience greater health impacts from air pollution exposure. The RCPCH calls on governments, local authorities, and key anchor institutions to act to protect the most vulnerable, who have the least power and resources to control their environments.
Monitoring air quality in schools is such a good idea. Children and young people spend the majority of their time in school anyway, so having a focus on it is super important.
RCPCH activity on the topic
More people should be taught about clean air.
The RCPCH has secured funding from the Clean Air Fund to expand our work on climate change and air pollution. We have convened a network of over 100 child health professionals advocating for clean air locally and nationally, mobilised international paediatric speak with one voice, and delivered webinars and conference sessions on air pollution and its impact on child health.
We are showcasing best practices in tackling air pollution by gathering case studies and reviewing air pollution clinics in London and Liverpool. Our project aims to amplify the voices of children and young people, with RCPCH&Us workshops actively engaging young participants.
We are also updating the paediatric curriculum to include air pollution and encourage engagement with our educational resources.
In October 2023, we published a toolkit supporting paediatricians to take action locally, regionally and nationally on child health inequalities and climate change.
Building on that, we are proud to introduce the Air Pollution Companion—a comprehensive, one-stop resource designed to help integrate air pollution knowledge into clinical practice. Developed by the Clean Air Fund Partnership team, including three Clinical Fellows and RCPCH policy experts, the Companion helps users build their knowledge, communicate effectively with patients, and advocate for change.
- 1RCPCH (2024), RCPCH &Us Voice Bank, London: RCPCH (unpublished, available via and_us@rcpch.ac.uk)
- 1GBD 2021 Risk Factors Collaborators, 2024 ‘Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021’ Lancet 403:2162–2203
- 1RCPCH (2024), RCPCH &Us Voice Bank, London: RCPCH (unpublished, available via and_us@rcpch.ac.uk)
- 2
- 2Health Effects Institute, 2024. ‘State of Global Air 2024. Special Report.’ Boston, MA: Health Effects Institute.
- 2
- 2
- 2
- 2
- 2
- 2
- 3Fuller G, Friedman S, and Mudway I, 2023 ‘Impacts of air pollution across the life course – evidence highlight note.’ Environmental Research Group, Imperial College London
- 3
- 4UK Health Security Agency ‘Statement on the differential toxicity of particulate matter according to source or constituents: 2022’. Available at https://www.gov.uk/government/publications/particulate-air-pollution-he… [Accessed 12 June 2024]
- 5Department of Health and Social Care. ‘Chief Medical Officer's annual report 2022: air pollution’
- 6Grigg J, 2021 'Air pollution and respiratory inequality: lessons from high-income countries', in Sinha I, Lee A, Katikireddi S, et al. Inequalities in Respiratory Health (ERS Monograph). Sheffield: European Respiratory Society
- 7Parliamentary Office of Science and Technology, 2023. ‘POSTnote 691: Urban outdoor air quality’ Available at: https://post.parliament.uk/research-briefings/post-pn-0691 [Accessed 12 June 2024].
- 7
- 7
- 8Taylor M and Duncan P, 2023 ‘Choke Point’ The Guardian Weekly (analysis of data from the Expanse project) Available at https://www.theguardian.com/environment/2023/sep/20/revealed-almost-eve… [Accessed 12 June 2024]
- 9Department for Environment Food & Rural Affairs ‘Accredited official statistics Nitrogen Dioxide (NO2) Updated 30 April 2024’ Available at: https://www.gov.uk/government/statistics/air-quality-statistics/ntrogen… [Accessed 12 June 2024]
- 10Royal College of Paediatrics and Child Health, 2020 ‘The Inside Story: Health effects of indoor air quality on children and young people’
- 11Semple S, et al. 2012. ‘Contribution of solid fuel, gas combustion, or tobacco smoke to indoor air pollutant concentrations in Irish and Scottish homes’ Indoor Air 22: 212-223
- 12Kantar, 2020. ‘Burning in UK homes and gardens: Research report.’ Burnright. Defra.
- 13Department for Environment Food & Rural Affairs and Department for Transport, 2017 ‘UK plan for tackling roadside nitrogen dioxide concentrations: Detailed plan’
- 14Bath and North East Somerset Council, 2023 ‘Bath Clean Air Zone: Interim Monitoring Report January to June 2023’
- 15Greater London Authority, 2024 ‘London-wide ultra low emission zone - six month report’
- 16IPR Policy Brief, 2023 ‘Low Emission Zones improve air quality, physical health and mental well-being: Evaluating the impact of the Low Emission Zone (LEZ) and Ultra-Low Emission Zone (ULEZ) schemes in England’ Institute for Policy Research, University of Bath
- 17Royal College of Physicians and Royal College of Paediatrics and Child Health, 2016 ‘Every breath we take: The lifelong impact of air pollution’
- 18Ashworth M, et al. 2021 ‘Spatio-temporal associations of air pollutant concentrations, GP respiratory consultations and respiratory inhaler prescriptions: a 5-year study of primary care in the borough of Lambeth, South London’ Environmental Health 20:54
- 19Environmental Research Group, Imperial College London, 2022 ‘Health impact assessment of current and past air pollution on asthma in London’ Imperial College London: Projects
- 20Bongaerts, E et al. 2022 ‘Maternal exposure to ambient black carbon particles and their presence in maternal and fetal circulation and organs: an analysis of two independent population-based observational studies’ 6(10)E804-E811
- 21Lin LZ, Chen JH, Yu YJ, Dong GH. 2023 ‘Ambient air pollution and infant health: a narrative review.’ EBioMedicine. 93:104609
- 22Yu Z, et al. 2023 ‘Associations of improved air quality with lung function growth from childhood to adulthood: the BAMSE study’ European Respiratory Journal 61:2201783
- 23Sunyer J, et al. 2017 ‘Traffic-related Air Pollution and Attention in Primary School Children’ Epidemiology 2017;28(2):181-9.
- 24Newbury J, et al. 2019 Association of Air Pollution Exposure With Psychotic Experiences During Adolescence’ Jama Psychiatry 76(6):614-623
- 25Oudin A, et al. 2016 ‘Association between neighbourhood air pollution concentrations and dispensed medication for psychiatric disorders in a large longitudinal cohort of Swedish children and adolescents’ BMJ Open 6:e010004.
- 26Peralta A et al. 2022 ‘Quantile regression to examine the association of air pollution with subclinical atherosclerosis in an adolescent population’ Environmental International 164:107285.
- 27Farzan S, et al. 2021 ‘Childhood traffic-related air pollution and adverse changes in subclinical atherosclerosis measures from childhood to adulthood’ Environmental Health 20(1):44.
- 28Sørensen M, et al. 2023. ‘Effects of Sociodemographic Characteristics, Comorbidity, and Coexposures on the Association between Air Pollution and Type 2 Diabetes: A Nationwide Cohort Study.’ Environmental Health Perspectives 131(2):27008.
- 29Calderón-Garcidueñas L, et al. 2015 ‘Mexico City normal weight children exposed to high concentrations of ambient PM2.5 show high blood leptin and endothelin-1, vitamin D deficiency, and food reward hormone dysregulation versus low pollution controls. Relevance for obesity and Alzheimer disease.’ Environmental Research. 140:579-92.
- 30Fecht D, Fischer P, Fortunato L, et al. 2015. 'Associations between air pollution and socioeconomic characteristics, ethnicity and age profile of neighbourhoods in England and the Netherlands.' Environmental Pollution 198: 201-210.
- 31OECD, 2016 ‘The economic consequences of outdoor air pollution’ OECD Publishing, Paris. Available at: https://www.oecd-ilibrary.org/environment/the-economic-consequences-of-… [Accessed 26 June 2024].
- 32Awe YA, Larsen BK, Sanchez-Triana E, 2021 ‘The Global Health Cost of PM 2.5 Air Pollution: A Case for Action Beyond 2021’ (English). International Development in Focus Washington, D.C.: World Bank Group.
- 33Public Health England, 2018. ‘Estimation of costs to the NHS and social care due to the health impacts of air pollution: summary report.’ Public Health England/UKHSA.
- 34CBI, 2020. ‘Breathing life into the UK economy.’ Available at: https://www.cbi.org.uk/media/5539/2020-09-cbi-economics-caf-report.pdf [Accessed 26 June 2024].










