- What children and young people say
- Overview and teaching resource
- How paediatricians use this domain in their everyday practice - videos
- Parental decline for routine childhood immunisations - case study
- Patient presenting to acute paediatrics with incidental finding of obesity - case study
- Supervision session - video
- HEE health promotion toolkit
- Downloads
These resources are related to the curriculum domain, 5 - Health promotion and illness prevention. They were developed with current trainees and supervisors, RCPCH Officer for Health Promotion as well as children and young people.
What children and young people say
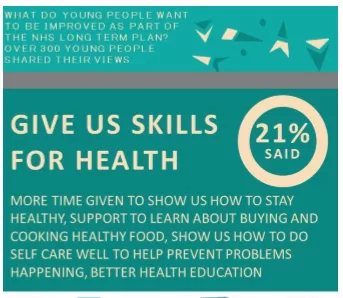
We asked CYP what keeps you healthy, happy and well? Here's some of what they told us...
- Interactive and memorable health information
- Health checks - for vulnerable groups and in secondary school
- Doctors understanding how to support good mental health
- More opportunities for parents and patients to talk to each other and getting advice from people with lived experiences of conditions...
When asked what was important for the next 10 years of the NHS, they want more time given to show how to stay healthy - from buying and cooking healthy food to doing self care well.
RCPCH &Us have shared their voices and views with the Children and Young People's engagement team on this curriculum domain.
Download RCPCH CYP flyer below
Overview and teaching resource
Underpinning the knowledge:
- Encourage health behaviours at all interactions
- Know the wider social determinants of health
- Understand the relationships between culture, economy, harms and risk
Our presentation, which you might use for a teaching session, explains the domain in more detail.
Download teaching presentation below
How paediatricians use this domain in their everyday practice - videos
Dr Max Davie, Consultant Paediatrician (former RCPCH Officer for Health Promotion), explains the importance of health promotion and illness prevention in everyday practice.
Dr Ravi Jayaram at Countess of Chester Hospital - explains why he thinks health promotion and illness prevention is important at all levels of training.
Dr Anya Wilson, a trainee based in Glasgow, provides easy examples of how health promotion and illness prevention can be developed across all levels of training.
The below case studies give examples of evidence that could be used to demonstrate contribution towards the domain learning outcome.
Parental decline for routine childhood immunisations - case study
It is important not to blame [the parents] but remain professional and be empathic throughout
Setting: General Paediatrics / Respiratory / Infectious Diseases
How did this situation arise?
A 3 year old child is admitted with a severe community acquired pneumonia with effusion, is spiking high fevers and has an oxygen requirement. Chest ultrasound demonstrates a large 5cm effusion requiring a chest drain and intravenous antibiotics. Bacterial culture of this pleural fluid has grown Strep pneumoniae serotype 6A. This serotype should be covered by the pneumococcal vaccine given as part of the routine childhood immunisation schedule.
On review of the history, you note that the child’s parents declined routine vaccinations.
What happened?
This is a very difficult time for the family as their child is acutely unwell with a serious respiratory illness. While the decision not to vaccinate one’s child would seem like an unusual decision to medical professionals, parents usually believe that they are acting in their child’s best interests and generally don’t do this to risk harm to their child.
It is important to discuss the bacteriology results with the parents, highlighting that this was a potentially preventable infection. Most parents would feel very guilty in this scenario therefore it is important not to blame them but remain professional and be empathic throughout.
Explore why the family declined routine immunisations – was this due to misconceptions about the safety of immunisations or perhaps this was due to cultural, social or religious factors? Whatever the reason, provide the parents with the most up-to-date information about vaccinations, address any safety concerns and help them to make a more informed decision. Allow them to reconsider consenting to vaccinations and if possible, administer first set of immunisations pre-discharge. Update the GP and health visitor.
How did this support your development?
This scenario helps to develop communication skills in providing health advice in a non-judgemental manner and supporting families to make informed public health decisions.
Any practical tips?
You may come across many families who choose not to vaccinate their children during your training and often this information may have nothing to do with the child’s presenting complaint. As paediatricians we must remain professional throughout and ensure that families are making informed decisions based on best evidence by providing them with appropriate information.
Patient presenting to acute paediatrics with incidental finding of obesity - case study
Consider the timing of these interventions
Setting: Paediatric on-call rota
How did the opportunity arise?
You are the paediatric ST4 working the night shift at a busy district general hospital. Your GPST1 colleague has just seen a nine-year old boy with difficulty breathing and has made an appropriate initial management plan for the acute problem. As part of your discussion about the case, she informs you that the patient has a body mass index of 30 and she is concerned this may be impacting on his health. She has also noted that both parents are overweight.
What happened?
As the senior clinician on duty you need to prioritise patients with regard to the available resources. The immediate problem for this patient is his respiratory compromise which needs to be appropriately managed in the first instance.
It may, however, be reasonable to discuss issues such as excessive weight or healthy eating at a later date or time. This could be done on the morning ward round, for example. It may also be helpful to involve other professionals such as dietitians who can assist with offering advice on healthy eating.
How did this support your development?
Such a scenario is not uncommon in paediatrics and represents a valuable opportunity to practice holistic medicine. It is important to offer families and children realistic options and to be open and honest with them about health concerns when they are recognised as such.
Excessive weight is linked to multiple co-morbidities therefore effectively addressing it at an early stage is important.
Any practical tips?
Consider the timing of these interventions, for example it may not be appropriate to discuss with the patient who presents overnight. Broaching the subject of somebody’s weight is often challenging and may lead to difficulties with the doctor-patient-family relationship.
The excellent trainee will however become adept at these consultations. The aim is to suggest ways to mitigate this problem, for example creating a specific pathway for such patients to facilitate the discussion and therefore help patients and families to make progress.
Supervision session - video
This film is designed to help supervisors and trainees work with the new curriculum during their supervision sessions.
HEE health promotion toolkit
The HEE Health Promotion toolkit is available in the downloads box at the bottom of this page. This is a guide to support the evidencing of this curriculum domain.
Special thanks and acknowledgement to Dr Elise Weir and Dr Rupert Ellis, also to all who contributed in providing the content for this domain.