The Workforce team conducts a survey of new CCT (Certification of Completion of Training) and CESR (Certificate of Eligiblity for Specialist Registration) holders in paediatrics, approximately one year from their certification date. Below, read our key findings from the 2017 cohort study, and download the report below.
Last modified
29 November 2019
Post date
26 September 2019
Table of contents
Actions and recommendations
The RCPCH will:
- Investigate why newly qualified paediatricians who gained their Primary Medical Qualification in a non-UK country report having to apply for more jobs before successfully obtaining a consultant post than those who graduated in the UK.
- Continue to expand the offer of leadership and management training for newly trained paediatricians, such as the Stepping Up programme. Continue to expand the offer of webinars, podcasts and other learning methods that can be easily accessed for trainees.
- Support the career aspirations of newly qualified paediatricians to get involved in medical education, develop a special interest, engage in quality improvement and undertake more research/academic work.
Summary
- There is a significant difference in the number of job applications required of UK educated doctors compared with non-UK educated doctors. Among the class of 2017, doctors who completed their primary medical education in the UK sent an average of 1.6 applications before being appointed to a consultant post compared with 2.5 applications among doctors who graduated in a non-UK country. There was no meaningful difference between the number of applications made by men and women prior to successful appointment.
- It’s taking longer to train paediatricians. The time taken between registration on the GMC register and CCT qualification has increased about 1.5 years. In 2011 it took the average doctor 9.8 years from the start of training to be certified as a paediatrician whereas it now takes an average of 11.3 years. Note that this includes time taken out for parental leave and other out of programme activities. Despite the increased time spent in training the vast majority (81%) felt the length of training was about right.
- The use of the grace period is declining. As recently as 2011, 43% of those surveyed used their grace period before taking up a consultant position. Since then, the number of doctors using this period has declined significantly and now stands at 21%.
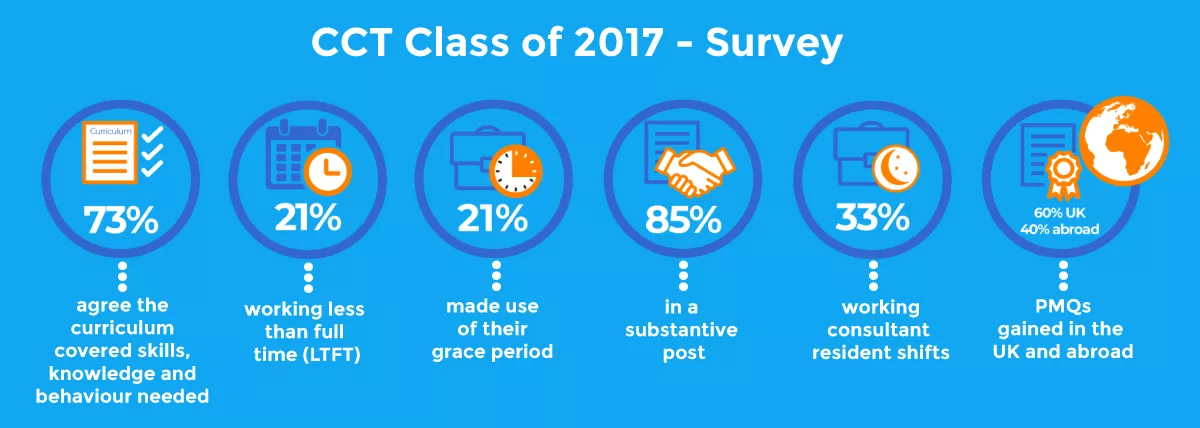
Key figures
- 85% of respondents were in a substantive post.
- 60% gained their PMQ (primary medical qualification) in the UK, 40% obtained their PMQ abroad.
- 21% were working less than full time (LTFT). 16% of respondents working full time would rather work less than full time.
- 21% made use of their grace period. Reported use of grace period has declined from 43% in the 2011 cohort to 21% in the 2017 cohort.
- 33% of respondents work consultant resident shifts.
- 73% either agreed or strongly agreed that the paediatric curriculum covered the depth and breadth of skills, knowledge and behaviour needed in their current role.