Read our summary here, or download the full report and appendices at the bottom of this page.
Background
Epilepsy12 was established in 2009 and has the continued aim of helping epilepsy services, and those who commission health services, to measure and improve the quality of care for children and young people with seizures and epilepsies.
The audit is commissioned by the Healthcare Quality Improvement Partnership (HQIP) as part of the National Clinical Audit and Patient Outcomes Programme (NCAPOP) and is delivered by the Royal College of Paediatrics and Child Health (RCPCH).
Epilepsy is the most common significant long-term neurological condition of childhood and affects an estimated 112,000 children and young people in the UK. Epilepsy12 seeks to help improve the standard of care for children and young people with epilepsies.
To do this, the audit collects and processes patient data. This information is used by the audit to highlight areas where services are doing well, and also identify areas in which they need to improve.
In 2022, a further contract was awarded to the RCPCH to deliver the audit up to 31 March 2025.
Epilepsy12 has seen considerable variation in the ability of different Health Boards and Trusts in England and Wales to provide adequate workforce time and resources to participate in the national audit. This has been particularly challenging throughout the COVID-19 pandemic.
We would like to thank the epilepsy services for their continued efforts to both provide care to children and young people with epilepsies throughout the pandemic, and to improve this care by participating in the audit. We recognise the dedication to children and young people with epilepsy that has driven audit data submission and quality improvement activities this past year. However, gaps in both clinical and organisational audit data indicate that some services had to suspend their activities to focus on maintaining core clinical duties.
Executive summary
Epilepsy12 is the national clinical audit of seizures and epilepsies in children and young people for England and Wales. There are three main elements to Epilepsy12 which are included in the annual report:
- A clinical audit of children and young people newly diagnosed with epilepsy in the ‘cohort 3’ patient group. These patients had their first paediatric assessment between 1 December 2019 and 30 November 2020. The audit then follows the cohort for 12 months of subsequent care.
- An organisational audit of paediatric epilepsy services, focusing on services and workforce at Trust/Health Board level, as they were at November 2021. At this time the NHS was dealing with a significant surge in COVID-19 cases and hospitalisations in England and Wales.
- Quality improvement activities and projects related to the audit. The annual report contains case study examples from NHS Trusts/Health Board, our Epilepsy Quality Improvement Programme and the Epilepsy12 Youth Advocates, showing ways services have been working together to make lasting improvements in care.
An updated version of the 2022 annual report has been published in November 2022. Epilepsy12 reports 12 'Performance Indicator' measures. You can find the results from the last three cohorts below:
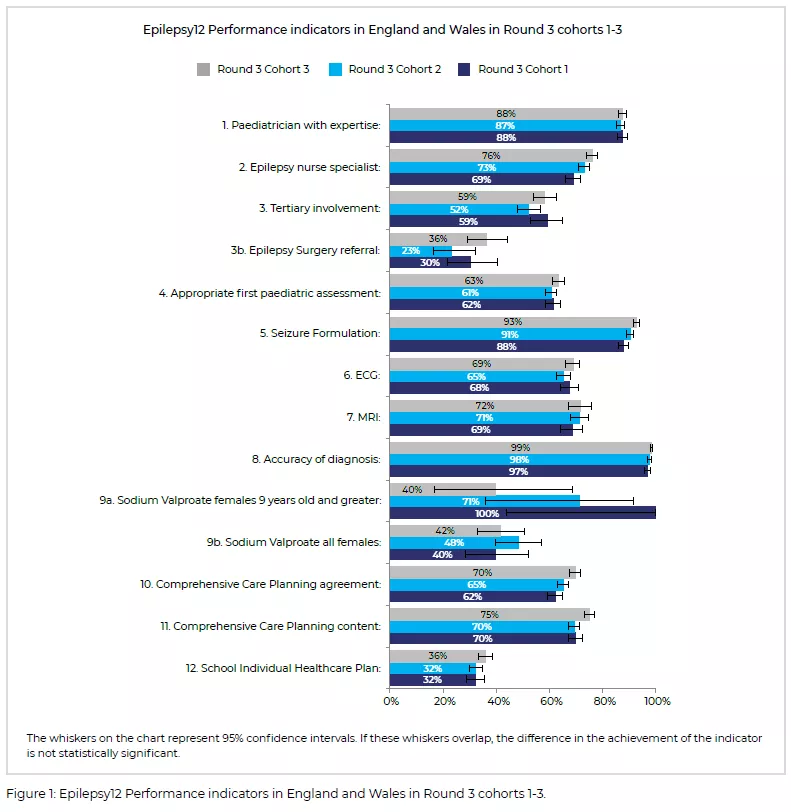
Overall, the results for the three cohorts are similar, which highlights both consistent areas of strength as well as continued scope for improvement in aspects such as input from specialists or tertiary services, comprehensive care planning and links to school epilepsy care plans.
Key messages
There was evidence of wide-spread use of comprehensive, individual care planning for children with epilepsy. Most care plans were agreed and updated. The proportion of plans which contained all the required elements also increased to 75% (1487/1974) in cohort 3.

There was evidence of increased joint-working to support young people to transition to adult services but the available support for patients varied considerably between services: 65% (75/115) of Health Boards and Trusts reported having an epilepsy outpatient service where there is a presence of both adult and paediatric professionals.

There was an increase in children and young people waiting more than 16 weeks for an initial Electro-encephalogram (EEG) in cohort 3 (10%, 191/1974). NICE Quality Standard 27 (statement 2) states that children and young people having initial investigations for epilepsy undergo the tests within 4 weeks of being requested.

Research suggests there is a higher incidence of mental health problems among children and young people with long term conditions, but very few of the epilepsy patients had an identified mental health condition (5%, 53/1124). Few epilepsy services could provide co-located mental health provision as recommended within the Best Practice Criteria (18%, 12/115).
Some children and young people with epilepsy may be missing out on, or having delayed referral to, epilepsy surgery assessments. 36% (49/135) of children and young people diagnosed with epilepsy who met surgical referral criteria had a referral for surgical evaluation during their first year of care.
Results by Health Board / Trust and regional network
Our detailed results spreadsheets cover the Round 3 clinical audit data for cohort 3 and the 2021 organisational audit results - download the MS excel spreadsheets below.
In the first tab, 'Information', you can see the 10 topics covered in each audit. You can filter each worksheet to view and compare data for one or more NHS Health Boards/Trusts, or Regional Paediatric Epilepsy Networks, or you can view for all units in England and Wales.
The audit measures that relate to the national report's key findings are highlighted in blue columns.
Specific Health Board / Trust level reports have been shared with the Epilepsy12 Designated leads by email.
Contact
The Epilepsy12 project team members are available to respond to any related queries at epilepsy12@rcpch.ac.uk or on Tel: 020 7092 6056 / 6157 / 6161









