About the survey, our quick read and full reports
We invited College members who were either current postgraduate doctors in training (PGDiT) who plan to obtain their Certificate of Completion of Training (CCT) within the next 18-24 months or doctors who had completed their CCT within the past five years to complete our survey in spring 2025.
Our reports present the findings. You can view our quick read below or in a new browser tab. For detailed information, please download the full report at the bottom of this page.
- Background to the survey
-
From 2011 to 2017 (published in 2019), we conducted annual surveys of paediatricians who had recently completed their specialist training, capturing information such as location, grade and number of hours worked.
We paused this work in 2019. We resumed in 2025 to explore the rapid changes over past years, such as the COVID-19 pandemic, our updated training curriculum, increased prevalence of flexible working and health sector pressures.
This survey was open from 8 April to 20 May to College members who were either: current postgraduate doctors in training (PGDiT) who plan to CCT within the next 18-24 months; or doctors who had completed their CCT within the past five years.
Topics covered were past and current training, including training length, location, pattern. Of current PGDiT, we asked about preparation for a consultant role, changes in training subject and location and information about transitioning. Of recently qualified consultants, we asked about the first role post-qualification and on transitioning into a consultant role.
Key findings
- More info on key findings
-
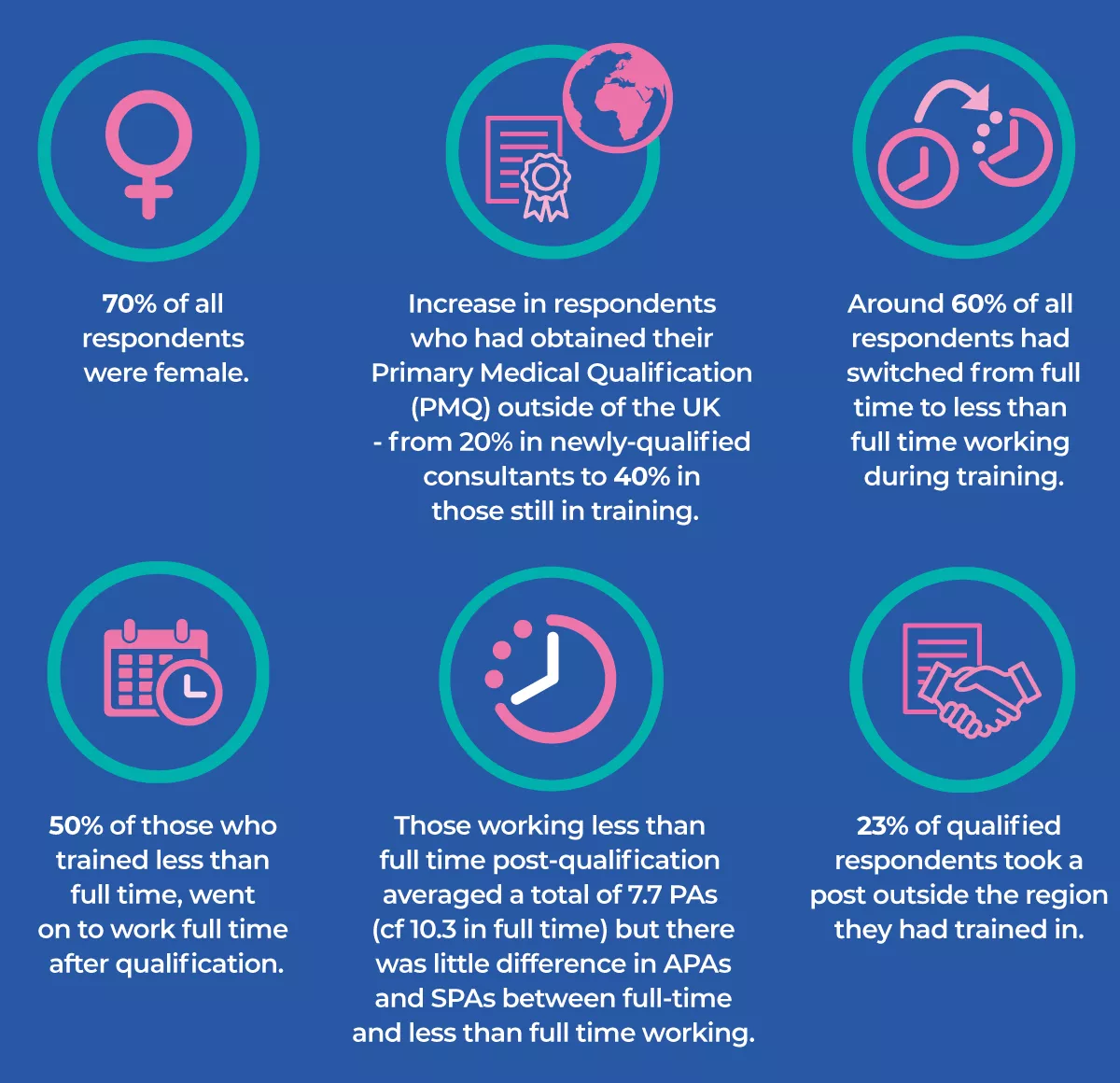
- 70% of all respondents were female while 40% of pre-qualification respondents had obtained their PMQ outside of the UK.
- 61% of pre-qualification and 52% of post-qualification respondents undertook less than full time (LTFT) training with 60% having switched during training; this was shown to be happening earlier in the training pathway.
- Of those who trained less than full time, around half went on to work full time after qualification.
- Full time consultants were working an average of 10.3 PAs compared to 7.7 PAs in LTFT, but there was little difference in APAs/SPAs.
- 74% of post-qualification respondents were working in substantive consultant roles, while nearly a quarter of qualified respondents intended to apply for a new role, the majority to obtain a substantive role.
- 23% took a post outside the region they had trained in.
- Over 50% of post-qualification respondents indicated an intention to decrease PAs.
Conclusion
This survey provides a window into the changing way paediatricians choose to train and work when they enter the specialist register. It gives insight into working patterns, first roles and the training experience.
Overall, this survey highlights a need to carefully map training posts to future service needs within a geographical area enabling post-qualification paediatricians to work close to the region in which they have trained and within their desired clinical area.
- Discussion
-
- The demographic composition the workforce had not changed significantly in recent years with the majority female and an average qualification age of 40 despite moving to a competency-based training programme and the option of accelerated training.
- The biggest change over the last decade is the number of paediatric doctors choosing to train less than full time (LTFT). This was mirrored by the latest GMC National Training Survey, which demonstrated a significant increase from 24.9% to 59.7% over the last decade .
- We also saw an earlier shift to LTFT training from ST4-7 to ST3-6, which may reflect a general change in LTFT being regarded as the ‘norm’ in addition to the ST3 pay increment suggesting greater emphasis on wellbeing.
- A quarter of respondents switched from training LTFT to working full time once they had qualified reflecting that they do not feel the need to work LTFT to maintain a work-life balance. Several factors may feed into this choice, such as, reduced unsocial hours as a consultant, reduced burden of not having to document progress in training, more flexibility in place of work, allocated time in job plan to complete administrative tasks, increased satisfaction and recognition in work delivered.
- The average number of PAs for FT and LTFT have not significantly changed over the last ten years. However, average number of SPAs allocated has increased, particularly in those working LTFT and as such the overall increase in LTFT, SPA time and corresponding decrease in DCC (within the same overall PA time), may explain the recent expansion of consultant workforce.
- Consultants are in general working in the clinical and geographical area in which they trained. However, with a lack of available posts being the main driver in changing roles and the fact that fewer than 10% of PGDiT had secured a consultant role, this may be an early indication that ratio of applicants to advertised post is increasing and more paediatricians will not directly enter a consultant post following qualification.
- Consideration needs to be given as to how posts are advertised so as not to prejudice applications from those wishing to work both FT and LTFT while job plans need to factor in time required to deliver necessary DCC alongside SPA considering how consultants can work collaboratively to ensure continuity care, job satisfaction and sustainability within the workforce, irrespective of the pattern of working.
If you have any questions about this project, please email us at workforce@rcpch.ac.uk.









