- Introduction
- Responsibility for training at a national level
- Responsibility for training at a regional level
- RCPCH role in training
- GMC role in training
- Employing Trust role in training
- Patient safety and risk issues - escalation
- Staffing issues
- Training and educational issues
- Morale and team working
- Sleep
- Less than full time working and returning to work
- Working conditions - rotas and contracts
- Education and training
This page was written in summer 2019 by Natalie Bee, Ollie Bevington, Julie-Ann Collins, Emma Coombe, Sian Copley, Kathryn Cox, James Dearden, Hannah Jacob, Claire Mathews and Rachael Mitchell on behalf of the RCPCH Trainees’ Committee. The Training & Quality team periodically reviews this page to ensure it is up to date. If you have any suggested edits, get in touch with us on training.services@rcpch.ac.uk.
Introduction
This web page is intended to be viewed alongside the Training Charter, a set of standards that all Heads of Schools, Training Programme Directors and training units are encouraged to proudly sign up to as a commitment to providing high quality training. It also complements the formal RCPCH Training Guide.
We'll highlight aspects of your working life that are overseen by different bodies, including the Royal College of Paediatrics and Child Health (‘the College’), the Deanery/Local Education and Training Board (LETB)/ Health Board and your employing Trust.
As a trainee, it can be confusing to work out who has ultimate responsibility though incredibly important; understanding this will allow you to discuss new ideas and raise concerns, where necessary, with the relevant body. Following is a brief explanation and more information can be found in the Gold Guide.
Responsibility for training at a national level
The health ministers are responsible for policy on medical education, reporting to the Secretary of State for Health & Social Care.
NHS WTE (previously Health Education England), NHS Education for Scotland (NES), The Northern Ireland Medical and Dental Training Agency (NIMDTA) and Health Education and Improvement Wales (HEIW) are the four bodies that support the delivery of healthcare and health improvement to the patients and public of their countries. This includes leading on workforce planning, medical trainee recruitment and accountability for outcomes achieved by education and training.
Perhaps most importantly, they also support training locally. In England this is done through Local Education and Training Boards (LETBs), which hold and allocate funding for the provision of education and training and commission education and training on behalf of member organisations. In the devolved nations, a similar process exists, but these are not called LETBs.
Responsibility for training at a regional level
Within each geographical area, Training Programme Directors (TPDs) are responsible for paediatric specialty training programmes, overseen by the Heads of School of Paediatrics. They plan training programmes based on the needs of the trainees, support educational supervisors and contribute to the ARCP (annual review of competence progression) process.
The Postgraduate Deans are responsible for the ARCPs and act as the Responsible Officer, making recommendations for revalidation to the GMC (General Medical Council) for each trainee. (For non-training grade doctors, the Trust, usually medical director or designate, rather acts as the Responsible Officer). There is more guidance from NHS WTE and Medical Education Leaders UK.
RCPCH role in training
The RCPCH serves a number of functions, including advocacy for children & young people, health policy and supporting paediatricians. You can read more about our aims on our College strategy page.
Particularly relevant to trainees, the College develops the postgraduate curriculum (RCPCH Progress+) and methods of postgraduate assessment (assessment strategy, including exams, workplace based assessments (WPBAs) and the assessment undertaken in later training, RCPCH START).
The College works closely with Heads of School to ensure quality training is delivered locally, although ultimately the control lies with local education providers in each region. College representatives also sit on ARCP panels.
What about trainee representation at the College?
The RCPCH Trainees Committee is a group of trainee representatives who are there to represent your views as trainees about issues that matter to paediatricians in training. There are regional representatives from each area across the UK, as well as subject representatives who sit on all major committees.
Have a look at the Trainee Committee page for more information, for contact details for specific reps, and how you can get involved.
GMC role in training
The GMC (General Medical Council) works to protect patients and the public by ensuring quality medical education and practice across the UK. Its main roles are:
- Overseeing medical education and training (e.g.by approving the Progress+ curriculum developed by the College)
- Setting standards for doctors in training and throughout their careers
- Deciding which doctors are qualified to work in the UK and acting to prevent a doctor putting patient safety at risk
Employing Trust role in training
Resident Doctor contracts are made and held by individual NHS employers, such as Trust or Health boards. Consequently, employers are distinct from organisations responsible for educational provision. However, the Gold Guide states, ‘healthcare organisations that provide training placements should explicitly recognise that supervised training is a core responsibility, to ensure both patient safety and the development of the medical workforce to provide for future service needs.
The employing Trust has a responsibility to deliver training to the standard required by the GMC; the Postgraduate Deans and LETBs have a responsibility to monitor the quality of education delivered by Trusts and taking remedial action, when Trusts fall below the required GMC standards.
Next we offer some guidance and signposting when there are problems in training.
Patient safety and risk issues - escalation
There may be times as a trainee that you have concerns about patient safety, staffing or the quality of your training. This section is intended to outline what you can and should do and what you can expect from your employing organisation.
What should my training centre do?
Training centres should have a policy in place for raising patient safety issues. These will vary depending on the type and size of Trust/ Health Board and may include:
- How to raise an initial concern
- Expected response method and time frame of a response
- Method of further escalation if no action has occurred
This policy should be easily available to all members of staff and highlighted to trainees during induction.
What should I do?
- Raise all patient safety issues, in a timely fashion, through the correct pathway
- Actively participate in quality improvement – to help resolve patient safety issues raised
- Have medical indemnity insurance – and consult them if you are involved in an incident
Staffing issues
Staffing is a specific safety concern, which is unfortunately an ongoing problem in paediatrics and may require specific escalation.
What should my training centre do?
All training centres should have a plan in place for dealing with both long term rota gaps and emergency short staffing.
Long term plans should include:
- Who is responsible for trying to fill gaps, for example service managers and consultant in charge of the rota
- What methods are used to fill gaps – for example, contacting staff lists and using locum agencies
- When other actions would be considered – for example, reducing elective care and asking other departments to reduce workload
Emergency plans should include:
- How they will try to fill gaps
- How the shortage will be reported and by whom
- How safe staffing levels will be determined and by whom
- Which other departments will be informed and how
It may include roles to be taken over by other departments (for example, the midwifery team to assist with new born examinations) or when a consultant would need to stay on site.
What should I do?
- Give as much notice as possible for periods out of work and for short notice absences
- Assist departments with assessment of workload and staffing requirements
- If last minute cover is required for a shift and you are not working, consider if you could help out; this should not be at the expense of your own rest breaks and you should not feel pressured to cover
- If you are working outside of your agreed work plan, complete an exception report
Training and educational issues
Training issues are slightly different, as they are not acute patient safety issues and therefore will require different escalation.
What should a training centre do?
See the Training Charter for more information on what Heads of School of Paediatrics have acknowledged. This includes:
- Provide all trainees with an educational supervisor with up to date training in educational supervision
- Work to facilitate training as detailed in individual’s work plan or personal development plan (PDP)
- Provide a forum for trainees to provide feedback, for example trainee meetings.
- Ensure trainees are aware of how to escalate training issues – for example, educational supervisor, College tutor
What should I do if I have training or education issues?
- If on a 2016 contract (see section on working conditions and contracts), engage with the workplan process to detail training requirements
- If on a 2002 contract– engage with the PDP to detail training requirements
- Attend and actively engage in trainee feedback sessions
- Raise any training issues as early as possible with your training centre - for example, Educational Supervisor or College Tutor
Deaneries/ LETBs are primarily responsible for training. If a local issue is not adequately addressed by the College Tutor, escalation should be through the Training Programme Director in the first instance, then the Head of School.
It is also important to raise such issues with your Regional RCPCH Trainee Representatives whose contact details are on the Trainee Committee page. This allows trainee reps to collate more widespread issues and they may be able to share solutions from other regions or suggest other avenues for support.
Morale and team working
Recognise the everyday excellence in departments and share learning from brilliance to keep it up!
Often the teams in which we work can make a huge difference to our experience of a particular workplace. Here we give you some ideas for things you can do to improve morale and teamworking in your local paediatric department.
Key suggestions
Learning from excellence - Rather than only submitting incident forms when something goes wrong or there's a near miss, some hospitals enable staff to submit forms when things go well or something excellent happens. This can be really positive to recognise the everyday excellence in departments and share learning from brilliance to keep it up! Some departments will even have a newsletter or noticeboard with the names of those mentioned in learning from excellence reports.
Pastoral support - Trainees should have access to resources to support their health and wellbeing, for example a confidential counselling services, careers advice and support and occupational health services. One example is the Practitioner’s Health Programme, a free confidential programme for doctors and dentists with physical or mental health problems. It is primarily based in London, but does take referrals from elsewhere across the UK.
Clinical work
Debriefs - Everyone has stressful times both in and out of work, and often a chat among colleagues goes a long way to help. For significant events such as the death of a child, a formal debrief will be arranged - and it is often useful to have an informal debrief with colleagues to talk through what has happened, even just a busy evening on call. It’s important to look after yourself and each other - a post-nights breakfast with the team can help!
Mandatory meet-ups during ‘on-call’ shifts - This can take various roles. In some areas all members of the arrest team or obstetric theatre team will meet at the start of a shift to familiarise themselves with peoples’ names and roles. In a general paediatrics setting, handovers during a night shift can be a good opportunity to catch up with the rest of your team, regroup about which jobs are needed and help you plan breaks.
Use nurse in charge/ hospital coordinator to filter bleeps - Aside from emergency bleeps, the nurse in charge or hospital coordinator will often filter bleeps where there aren’t people to cross cover you. This can allow you to get a bleep-free break for some rest overnight, which is recognised to improve performance. For more information, see the Sleep section below.
Educational opportunities
Supervised Learning Events (SLE) clinics - Trainees often comment that it’s tricky to get SLEs done in busy departments. Some departments have set up different ‘SLE clinics’. For example, some will have a consultant supervising a trainee-led clinic and completing a mini CEXs or CBD. Others involve a consultant having an afternoon dedicated to SLEs - you can book a slot and do a relevant SLE. If your department doesn’t already have something like this, try approaching the consultants to ask about setting something up.
Use study leave to get clinic time or a career taster - All trainees can take personal study leave days. A good use of these can be to go to specialist clinics you otherwise wouldn’t get to, or to do a taster week in a sub-specialty.
Protected teaching - In some areas there are protected Deanery-wide teaching days. Attendance is mandatory unless on nights or annual leave and consultants will expect you to attend on your relevant day (for example, ST1 teaching on second Wednesday of the month) with no need to request study leave. This culture shift makes it much easier to attend teaching and is also a great opportunity to meet with your peers.
Administrative ideas
Leave requests - Have you ever struggled to work out who to get in touch with at your new hospital trust to make leave requests? In some regions the trainees have compiled lists of who to get in touch with at each hospital. Maybe talk to your fellow trainees and start putting together a list that can then be easily updated each year.
A regional rep committee - Each region has a regional rep who is on the RCPCH Trainees’ Committee and can represent you nationally on that. Most regions also have internally appointed reps (eg Core and Specialty level reps), and some regions have formed very successful regional rep committees that coordinate both work-related and social events (including the very successful PAFTAs, or paediatric trainee awards). If your region doesn’t have one, why don’t you approach your regional rep and TPDs and get one going?
Induction - If there was something missing from your induction, let your consultants know so they can make sure it goes into the next induction. It is also really important that you can attend induction. In many places consultants will cover shifts themselves to allow you to attend or use locums where possible.
Other morale boosting initiatives
Hello my name is… - This is a campaign lots of people are familiar with through the work of Dr Kate Granger, an elderly care doctor who after receiving a cancer diagnosis and noting that often staff did not introduce themselves created this campaign - you will see staff with hellomynameis… badges all over the place and a huge campaign on Twitter!
Using first names for consultants - It is a well-recognised phenomenon that flattens the hierarchy between postgraduate doctors in training and consultants, leading to greater patient safety and better team working.
Group socials/ Bake offs - Everyone loves cake! Lots of departments run Bake off competitions creating opportunities for socialising and bonding between teams. Socials are a great idea to get everyone to know each other outside of work, creating better working relationships. Try organising one in your new department.
Sleep
Out-of-hours, specifically night shift work, form a significant proportion of any paediatric or neonatal rota. This section signposts to available resources and evidence-based advice to help your body adapt to working these unnatural shift patterns.
Key components of this are also included in the Trainee Charter to outline how best to provide necessary patient care and service provision, while looking after the wellbeing of staff undertaking night shifts.
You can find out more about sleep, breaks and wellbeing in this article by Dr Michael Farquhar.
Why is fatigue important?
- Impacts on patient safety - This is the headline and why the GMC have started to take an interest in the level of exhaustion in trainees. Tired doctors perform less well, make riskier decisions, deal with novel situations more slowly and have impaired learning.
- Impacts on personal safety - There is an increased risk of vehicle accidents. Sleep deprivation is akin to raised blood alcohol level.
- Impacts on personal health - Mental health and cardiovascular risks are greater in shift workers.
What can you do to improve your sleep?
- Ensure good core sleep - Prioritise quality sleep when you are not working night shifts, and minimise your “sleep debt”.
- Ensure a good sleep environment - Make sure it's cool, quiet and dark. Invest in blackout blinds, ear plugs, face masks and fans to optimise your room.
- Ensure there are good core sleep routines and habits - Keep electronic devices such as phones out of the bedroom, and ensure you aren’t disturbed by housemates/visitors.
What can you do to adapt to night shifts?
- Preparation - "Bank” extra sleep before the first night shift, and nap in the afternoon.
- Survival - Take 20-45 minute naps during your statutory breaks to counteract the effects of fatigue, keep work areas brightly lit, stay hydrated, try to eat healthily and use caffeine judiciously.
- Recovery - If you are too tired to drive, don't! Try to sleep immediately on getting home. Avoid alcohol, nicotine or sedatives. Optimise your daytime sleeping environment.
- Final night - Recover your sleep debt with a 1-2 hour nap before midday.
What must Trusts provide regarding sleep?
Rest break entitlements/ requirements are explored in further detail in this section. If you work in England, staff should have one 30-minute break for a shift greater than five hours, two 30-minute breaks for a shift greater than nine hours, and a third 30 minute break for night shifts lasting longer than 12 hours. Making sensible use of these rest periods to have restorative naps during a night shift is encouraged in many Trusts and shown to improve productivity. The newer requirements, regarding rest facilities, in the 2016 contract are in paragraphs 9 and 10 of schedule 13; terms and conditions as shown below. Providing a room for only a few hours is unlikely to put the doctor in a better position to safely travel home from a fatigue perspective.
"Where a doctor advises the employer that the doctor feels unable to travel home following a night shift or a long, late shift due to tiredness, the employer shall where possible provide an appropriate rest facility where the doctor can sleep. The hours when the doctor is resting in the hospital under these circumstances will not count as work or working time. Where the provision of an appropriate rest facility is not possible, the employer must make sure that alternative arrangements are in place for the doctor's safe travel home.
"Where a doctor is rostered to work on a non-resident on-call working pattern and is required to return to work during the night period and the doctor considers it unsafe to undertake the return journey home due to concerns over tiredness, the employer shall where possible provide an appropriate rest facility if requested where the doctor can rest. The hours when the doctor is resting in the hospital under these circumstances will not count as work or working time. Where the provision of an appropriate rest facility is not possible, the employer must make sure that alternative arrangements are in place for the doctor's safe travel home.
"An 'appropriate rest facility' can take two forms:
- A bedroom, of sufficient quality, provided directly by the employer
- An employer purchased hotel or B&B room in close proximity to the doctor's working site."
What should Trusts and departments provide regarding sleep?
- Education - Teaching and training within the department and at trainee induction to raise awareness of shift-work, fatigue and sleep
- Facilities - Easily accessible, appropriate rest areas and facilities adhering to a minimum standard, as outlined by AAGBI. Provide access to healthy, cooked food at all times of the day
- Sympathetic Rotas - Acknowledge the requirements for recovery time, and minimise frequent transition between night/day shifts
- Positive culture - Positive and active encouragement of use of rest periods to improve overall productivity and ensure patient safety. Support mechanisms such as Exception Reporting, when this is not being achieved
- Wellbeing support - Offer regular screening for shift workers for sleep disorders and other health issues associated with shift work
Resources
Dr Michael Farquhar, Consultant Paediatrician is a leading campaigner for the recognition of the importance of sleep, and you can see his advice in this article on this website.
The Association of Anaesthetists of Great Britain & Ireland (AAGBI) and Royal College of Anaesthetists (RCoA) have also produced extensive guidelines and resources regarding fatigue in postgraduate doctors in training.
- Fifteen minute consultation: problems in the healthy paediatrician – managing the effects of shift work on your health. M Farquhar. Arch Dis Child Educ Pract Ed 2017; 102:127-132
- Optimising sleep for night shifts. H McKenna. BMJ 2018; 360:j5637
- AAGBI Fight Fatigue Campaign
- British Medical Association - fatigue and sleep deprivation resources and the Fatigue & Facilities Charters
- Health and Safety Executive - Managing shift work
- Drowsy Driving
- Tuck Sleep
- Sleep Council
Less than full time working and returning to work
Paediatrics has a higher proportion of less than full time (LTFT) trainees than any other specialties. This section outlines the main issues around LTFT working and signpost you to resources that can provide more information.
The Gold Guide from July 2022 states that LTFT aims to:
- Retain in the workforce doctors who are unable or do not wish to continue their training on a full time basis
- Promote career development and work/life balance for doctors training in the NHS
- Ensure continued training in programmes on a time equivalence (pro rata) basis
A balance needs to be maintained between LTFT training arrangements, the educational requirements of both full time and LTFT trainees and service need.
What is the process for applying for LTFT training?
Applications should be made in writing to the LETB/ Deanery as early as possible using the locally agreed forms.
The LETB/ Deanery should inform the trainee of whether an application has been successful within three months. Where permission is not granted for LTFT working, an explanation should be given.
Trainees must apply in writing for any change in LTFT percentage working. There may be a delay in offering the requested percentage due to employment/training constraints. Information on the application processes should be readily available on NHS WTE/ LETB/ Deanery websites.
How do the working patterns of LTFT trainees differ?
Working patterns for LTFT should:
- Reflect the same balance of daytime working, on -call and out-of-hours work as their full-time colleagues, unless there is good reason not to. Either way, legal and educational requirements must be met
- Usually move between placements within rotations on the same basis as a full-time trainee
Trainees should not be excluded from particular rotations or educational opportunities on the basis of LTFT working.
What about access to study leave/budget?
LTFT are entitled to the same study budget as their full-time colleagues. Study leave is available on a pro-rata basis.
Where LTFT trainees undertake study leave or mandatory training which is not available at another time on their non-working days, they are entitled to time off in-lieu.
Statutory and mandatory training is not counted as study leave and is therefore taken in addition to the pro-rata allocation of study days.
Who can I talk to more about LTFT training?
Your Educational Supervisor and College Tutor are good places to start for advice. There is also a consultant LTFT representative in every LETB/ Deanery who provides a first point of contact for advice on LTFT training and will link with other regional reps.
Additionally, trainees can seek advice from the RCPCH LTFT trainee representative on the RCPCH Trainee Committee. Read more on the RCPCH LTFT webpage.
LETBs/ Deanery’s should maintain a list of LTFT trainees locally to allow information sharing for local and national issues relevant to LTFT trainees.
Return to work
Returning to clinical work after a period away for any reason can feel daunting. There are a several things that can help make this transition easier and there is guidance from GMC, BMA, NHS WTE and Academy of Medical Royal Colleges. They all say similar things and we have distilled their advice:
- Talk to your Educational Supervisor, ideally a couple of months before you return. You can discuss any worries you have, any specific requirements and plan the best way of you coming back to work. In addition, money has been allocated at a national level to facilitate safe and supported return to work after a period of absence for any reason. Your Educational Supervisor can work with you to think how best you might access this money and make use of it to make your return to work as smooth as possible.
- Write a ‘Return to work’ plan which can help you identify areas of strength and also areas of potential educational and practical need. This can be a useful starting point with your Educational Supervisor. If circumstances allow, ideally you should consider your return to work plan before you leave to ensure the process goes smoothly at both ends.
- Keeping in touch days – ‘KIT Days’ – You are entitled to up to 10 KIT days before you return to work after parental/adoption leave and are entitled to be paid at the basic daily rate for the hours worked.
- Consider a ‘return to acute clinical practice course’ – Most LETBs/deaneries are now running some form of course for those who have been out of acute clinical practice and this can be a great opportunity to discuss worries, practise using simulation and build confidence.
- Life Support Courses – Make sure your life support certificates (NLS, APLS, EPLS) are up to date. You can still claim funding from your study leave budget and count the day as a KIT day if on parental leave.
- Liaise with your rota coordinator – Ideally your first couple of weeks would be all in-hours working and speaking to your rota coordinator early can help ensure you are not put on nights in your first week.
- Attend Trust induction – These run fairly frequently and can save you the hassle of having to spend your first few days struggling with IT passwords and mandatory training.
- Speak to the Consultant on-call – Make sure that the people you are working with know you are returning from a period away from clinical practice. This will allow them to best support you in your first few shifts and help you feel more confident.
- Talk to Occupational Health – Depending on your reason for being away from clinical practice, it may be appropriate for you to have a phased return and for your employers to make reasonable adjustments to the way you work. Involving Occupational Health can help ensure that any health challenges you have are factored in to this planning.
Resources
- GMC Supporting those returning from a break in clinical work
- BMA Returning to clinical practice
- NHS England Supporting doctors returning to training
- AoMRC Return to practice guidance (PDF)
Working conditions - rotas and contracts
This section outlines key issues around working conditions and rotas with practical advice about where you can go for more specific advice.
What can you expect as a paediatric trainee from your rota?
If you are a BMA member, more detailed information is available in the Junior Doctors Handbook. Further information about contracts in England and the Devolved Nations can be found on the BMA website. The Gold Guide is also a valuable resource for all doctors in training.
What should happen before you start work?
If employed on 2016 Terms and Conditions (T&Cs) you can expect to receive a “generic work schedule” up to 8 weeks before commencing in post. This details the general rota pattern but may not have you allocated to a particular slot on the rota yet.
On 2002 T&Cs you can expect to receive a rota up to 6 weeks in advance of your start date.
On 2016 T&Cs you should receive the rota by then and also a personalised work schedule. This should detail your clinical responsibilities in the post, the educational experiences you should expect, including local and regional teaching, opportunities for clinic and other relevant training opportunities.
If you don’t receive these in a timely manner you should contact medical HR, the Guardian of Safe Working and the clinical lead of the department you’re rotating to.
What about booking annual leave?
Under both 2002 and 2016 contracts, your annual leave entitlement goes up after 5 years’ service working for the NHS.
In general, it helps to give a department as much notice as possible if you have specific dates you’d like to take your annual leave. You do not need to wait for a rota to be issued before you can request leave. This is particularly true for important life events like your own wedding.
Most departments operate a first-come first served approach to leave, and the exact mechanism for booking leave can vary from department to department - so try and find out what system the department operates before you start.
In general, all reasonable requests should be granted if you give more than six weeks’ notice. Fixed leave is allowed under 2002 contract but not the 2016 contract. If you’re having difficulty agreeing your leave then you can escalate to the Guardian of Safe Working if on the 2016 contract.
What should I do if I need to take sick leave?
If you are unwell and unable to work, you must notify your department as soon as you are able. If your sickness continues beyond three calendar days, you must inform your employer of the nature of your illness. You can self-certify your illness for up to seven days.
If you have more than 14 days leave (including sick leave and other types of statutory leave) in a training year then this may be taken into account when considering your progression at ARCP.
Rota Rules at a glance – 2002 terms and conditions
For those working under the 2002 terms and conditions, your protection regarding your working hours comes from the European Working Time Directive (EWTD) and the “New Deal” which dates back to 1991 but still forms part of the 2002 contract. The restrictions outlined in each of these do vary, but apply simultaneously so as to offer maximum protections to resident doctors.
Maximum hours of work
- Up to 48 hours a week on average (EWTD maximum)
- Up to 56 hours a week on average (New Deal maximum – for those opting out of EWTD)
Rest requirements
- You should have a minimum of 11 hours’ continuous rest in every 24-hour period (EWTD)
- You should have a minimum period of 24 hours’ continuous rest in each 7-day period (or 48 hours in a 14-day period) (EWTD)
- You should have at least 30 minutes’ continuous rest after approximately 4 hours continuous duty. Posts that do not comply with this rest requirement must be paid at band 3.
What happens if rota rules are broken (under 2002 T&C)?
When these restrictions are breached, the mechanism of flagging this with your employer is hours monitoring. Monitoring should occur every 6 months and during a representative period of work. The results of the monitoring should be made available to trainees 15 working days after the last day of the monitoring period. Data must be received from 75% of the monitored doctors for the result to be deemed valid.
Rota rules at a glance – 2016 terms and conditions
The rota rules and what to do if these are broken are different for the new 2016 contract. In addition to the protections within the contract, additional advice regarding rostering jointly agreed between NHSE and The BMA is available.
|
Rule |
Notes |
|---|---|
| Max 48 hour average working week. | A guardian of safe working hours fine will apply if this rule is breached. |
| Max 72 hours work in any 7 consecutive days. | A guardian of safe working hours fine will apply if this rule is breached. |
| Max 13 hour shift length. | On-call periods can be up to 24 hours. |
| Max 5 consecutive long shifts, at least 48 hours rest following the fifth shift. | Long shift - a shift rostered to last longer than 10 hours. |
| Max 4 consecutive long daytime/ evening shifts, at least 48 hours rest following the fourth shift. | Long evening shift - a long shift starting before 16:00 rostered to finish after 23:00 (a long shift starting after 16:00 will fall into the definition of a night shift. |
| Max 4 consecutive night shifts. At least 46 hours rest following the third or fourth such shift. | Night shift - at least 3 hours of work in the period 23:00 to 06:00. Rest must be given at the conclusion of the final shift, which could be the third or fourth. |
| Max 8 consecutive shifts (except on low intensity on-call rotas), at least 48 hours rest following the final shift. | Low intensity on-call - duty on a Saturday and Sunday where 3 hours, or less, work takes place on each day. Up to 12 consecutive shifts can be worked in this scenario provided that no other rule is breached. |
| Max frequency of 1 in 2 weekends can be worked. | Weekend work - any shifts/ on-call duty periods where any work falls between 00:01 Saturday and 23:59 on a Sunday. |
| Max frequency of 1 in 2 weekends can be worked (special exception for nodal point 2). | For one placement at F2 (typically emergency medicine), the definition of weekend work is any shift rostered to start between 00:01 Saturday and 23:59 on a Sunday. |
| Normally at least 11 hours continuous rest between rostered shifts (separate on-call provisions below). | Breaches of rest subject to time of in lieu (TOIL) which must be given within 24 hours. In exceptional circumstances where rest reduced to fewer than 8 hours, time will be paid at a penalty rate and doctor not expected to work more than five hours the following day. A guardian of safe working hours fine will apply in this circumstance. |
| 30 minute break for 5 hours work, a second 30 minute break for more than 9 hours; a third break for night shifts lasting more than 12 hours. | A guardian of safe working fine will apply if breaks are missed on at least 25 per cent of occasions across a four week reference period. Breaks should be taken separately but if combined must be taken as near as possible to the middle of the shift. |
What happens if rota rules are broken (under 2016 T&C)?
On the 2016 contract, if you work excessive hours, are unable to safely take breaks, or miss educational opportunities due to service pressures, the mechanism to record this with your employer is exception reporting. You should receive information with your induction telling you how to access an electronic means of submitting exception reports.
The way these reports are dealt with differs from trust to trust but usually they go to your educational supervisor and you can agree to be paid or take time back in lieu for excessive hours. This system is overseen by the Guardian of Safe Working which is usually a consultant in each Trust.
Education and training
This section outlines what you can expect from your education and training and details of who is responsible for what. There is also a Training Charter which training units are encouraged to sign up to.
General principles
- The GMC states that the environment and culture for education and training (E&T) should meet learners’ and educators’ needs, be safe, open, and provide a good standard of care and experience for patients.
- E&T should be a valued part of organisational culture - see the GMC Promoting excellence themes.
- Trainees should have protected time for learning, and for attending organised educational sessions, training days, courses and other learning opportunities to meet the requirements of their curriculum.
- In timetabled educational sessions, you must not be interrupted for service unless there is an exceptional and unanticipated clinical need to maintain patient safety.
- At certain levels of training, for certain placements or sub-specialties there are minimum standards for specific learning opportunities that should be available to trainees, for example the number of clinics that a trainee should attend. There is variation across the UK and it would be best to contact your regional representative to see if any standards exist in your region.
- Learners must have access to resources to support their health and well-being, and to educational and pastoral support, including: a confidential counselling services, careers advice & support and occupational health services.
Training programmes
- Whilst learners are responsible for their own learning and achieving the learning outcomes required by their curriculum, training programmes should be designed so that trainees can fulfil the requirements of their curriculum across a range of placement throughout their training.
- Learners must make care of patients their first concern and have a duty to follow the guidance in Good Medical Practice.
- Learners must have access to technology-enhanced and simulation-based learning opportunities within their training programme to enhance trainees’ learning and help fulfil ‘hard-to-reach’ portions of their curriculum
- If training in a subspecialty at Level 3, trainees should spend at least 70% of their time in their chosen speciality, with up to 30% providing acute unscheduled care, in order to achieve their subspecialty competencies.
- General paediatric and sub-specialty trainees should share the burden of out-of-hours care in an organisation, such that both groups have an equitable split of daytime and out of hours work.
- Training programmes should be designed such that no more than 33% of hours worked by all trainees should be in the delivery of emergency out of hours care.
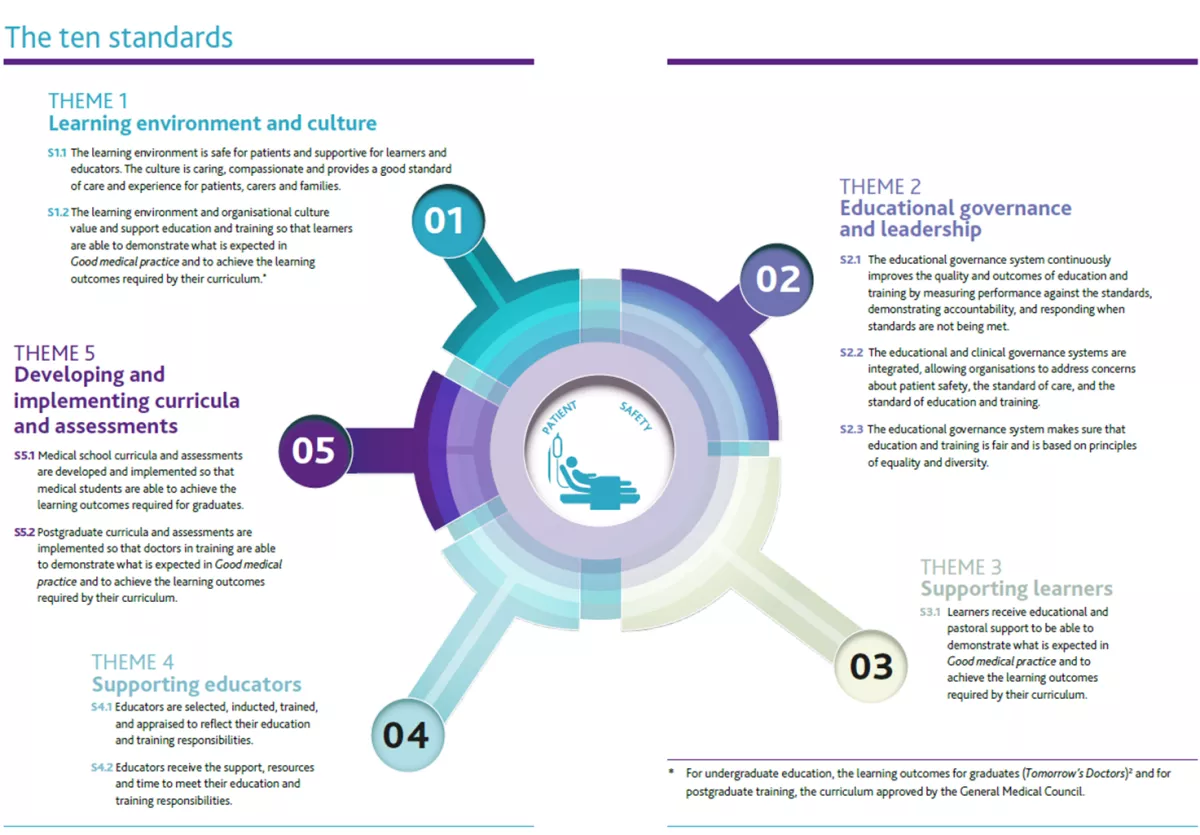
See the GMC's ten standards in the GMC Promoting Excellence document, or view the below image or download the image.
Supervision
- Learners must receive regular, constructive and meaningful feedback on their performance, development, and be encouraged to act on it. Feedback should come from educators, other doctors, members of the multi-professional team and, where possible, patients and families.
- The trainee should be supported by a dedicated Educational Supervisor, who should:
- have protected time for training of a minimum of one hour per week per trainee
- provide formative and summative feedback and support the trainee appropriately.
- In some places this may include having a supervisor for the duration of their core training.
- Trainees are expected to have clinical supervision all times by an identified individual. In practice, this is provided by the next most senior member of the team.
- Organisations responsible for managing and providing education and training must monitor how educational resources are allocated and used, including ensuring time in trainers’ job plans.
Assessments
- Trainees should take ownership, completing and reflecting upon a range of assessments in a timely manner throughout each placement, focusing on quality not quantity.
- Trainers should complete appropriate assessments as requested by a trainee in a timely fashion.
- Trainers should also look for ‘teachable moments’ and invite trainees to complete relevant assessments.
- For more information on assessments, see the RCPCH guide to Assessments.
There is lots of work being done to improve the flexibility of postgraduate medical training. RCPCH Progress+ will allow greater flexibility as it follows the GMC’s Generic Professional Capabilities, making it easier to transition between specialties.
We hope this supports your training. Do let us know via training.services@rcpch.ac.uk if you have any suggestions. And remember to contact your regional trainee representative for support where needed.