- Applying to paediatrics
- Registering for paediatric training
- Training fee
- Progress+
- RCPCH ePortfolio
- Progressing through training and ARCP
- Sub-specialty training
- Special interests (SPIN) modules
- Certification
- Possibilities in training
- Balance between general (acute) and sub-specialty training in specialty level paediatrics training
- Safe cover capabilities
- Your Trainee Committee
- Downloads
This guide complements the Conference of Postgraduate Medical Deans (COPMED) Gold Guide, which sets out the arrangements agreed by the four UK health departments for specialty training programmes.
You can also read our Trainee toolkit - by trainees, for trainees about what to expect from a training post with examples of good practice, as well as the Training Charter, a hallmark of high quality local training.
Applying to paediatrics
- After you complete your medical school and foundation years, you have the opportunity to apply to paediatric specialty training. This is done through competitive recruitment.
- Most trainees apply to and start at Core Level training, or ST1. Each full time equivalent training year is progressively labelled ST1 to ST7.
- Once recruited, you are appointed to a place of training run by a Statutory Education Board (SEB) for either England (NHSE), Wales (HEIW), Northern Ireland (NIMDTA) or Scotland (NES).
- Once in post, you are enrolled in a training programme and linked to an educational supervisor. This link is shown on RCPCH ePortfolio, our online assessment tool for all trainees.
About applying at ST1 and at ST3
Registering for paediatric training
- It is mandatory for paediatricians undergoing run-through training to register with RCPCH for training and become a member (normally on the Junior membership type).
- When you apply online for RCPCH membership, you can add 'training' to ensure you are given the correct fee category for appropriate ePortfolio access for a doctor in training.
- When you have been successfully appointed to a training post in the UK, we will contact you to apply as a Junior member (with training) of RCPCH. Once you've successfully applied, we'll set up your RCPCH ePortfolio.
How to apply for RCPCH membership
Training fee
Updated for the 2025 calendar year
There is a training fee for the work we do to support your training and for usage of ePortfolio. This is additional to your membership fee and to your exam costs. You can see detail in the below tables, depending on whether you entered training before or after 1 August 2019.
The training fee structure changed in August 2019 to reduce the costs at earlier stages of training and to more accurately reflect the costs of the services we provide.
Training and START fees in 2025 if you enter training BEFORE 1 August 2019
The below two tables shows the annual training fee and the START fee based on full time, run-through training for each training level for those entering training before 1 August 2019. The annual training fee for LTFT (less than full time) is 60% of that for full time, or £140.
| Training grade started (before 1 Aug 2019) | Training fee (per year) | |||||||
|---|---|---|---|---|---|---|---|---|
| ST1 | ST2 | ST3 | ST4 | ST5 | ST6 | ST7* | ST8* | |
| Begins at ST1 | £234 | £234 | £234 | £234 | £234 | £234 | £234 | £130 |
| Begins at ST2 | £234 | £234 | £234 | £234 | £234 | £234 | £130 | |
| Begins at ST3 | £234 | £234 | £234 | £234 | £234 | £130 | ||
| Begins at ST4 | £234 | £234 | £234 | £234 | £130 | |||
*After you complete START, your annual training fee reduces to £130 for the remainder of your training.
The START fee is the indicative fee based on payment contributions. For every £234 of the training fee, £97 goes towards START. For those starting later than ST1, the contribution will differ and the START fee will change. (The cost of START is adjustable where the training fee has not been received, regardless of which grade training you began. We will advise individually in such circumstances).
| Training grade started (before 1 Aug 2019) | START fee |
|---|---|
| ST1 | £268 |
| ST2 | £365 |
| ST3 | £462 |
| ST4 | £559 |
Training and START fees in 2025 if you enter training ON OR AFTER 1 August 2019
The below table shows the annual training fee and START fee based on full time, run-through training for each training level on or after 1 August 2019. The annual training fee for LTFT (less than full time) is 60% of that for full time, or £78.
| Training grade started (on or after 1 Aug 2019) | Training fee (per year) | |||||||
|---|---|---|---|---|---|---|---|---|
| ST1 | ST2 | ST3 | ST4 | ST5 | ST6 | START | ST8** | |
| Begins ST1 | £130 | £130 | £130 | £130 | £130 | £130 | £850 | £130 |
| Begins ST2 | £130 | £130 | £130 | £130 | £130 | £850 | £130 | |
| Begins ST3 | £130 | £130 | £130 | £130 | £850 | £130 | ||
| Begins ST4 | £130 | £130 | £130 | £850 | £130 | |||
**ST8 no longer exists since we introduced the Progress+ training programme in August 2023
How we use the trainee feee
- We maintain, develop and troubleshoot RCPCH ePortfolio.
- We administer registration and training enquiries, such as out of programme (OOP) and certification of completion of training (CCT).
- We provide support to our committees, including (but not limited to) Trainee Committee and TC Exec, a CSAC for each of the paediatric sub-specialties, Less than Full Time Committee, Training and Quality Board (TQB) and Heads of School.
- We develop the Progress+ curriculum, implement assessments, support on recruitment support and provide careers advice.
Refund for training fee
If you have paid a training fee and are eligible for a refund, we adopt a quarterly approach to refunds as determined by the membership fee refund and agreed by the RCPCH Executive Committee.
| Date resignation received | Refund of training fee |
|---|---|
| January, February, March | 75% |
| April, May, June | 50% |
| July, August, September | 25% |
| October, November, December | None |
Progress+
The RCPCH Progress+ curriculum has 11 domains, each with learning outcomes that capture the skills, knowledge and behaviours you'll need as a paediatrician. Progress+ has the same 11 domains as in the previous Progress curriculum, but outlines 11 training principles. It is a two-level training programme (rather than three levels as under Progress).
Progress+ curricula, syllabi and resources
RCPCH ePortfolio
As a paediatric trainee, you and your educational supervisor will use RCPCH ePortfolio (on the risr/advance platform, formerly Kaizen) to record learning in all its forms and settings, and to monitor progress through the curriculum. It is is mandatory for all run-through paediatricians in UK training posts.
Your ePortfolio:
- enables you to record assessments and development logs
- holds any personal development plans (PDPs) you wish to create
- is where your Local Education and Training Board (LETB) or deanery submit your Annual Review of Competence Progression (ARCP) outcomes.
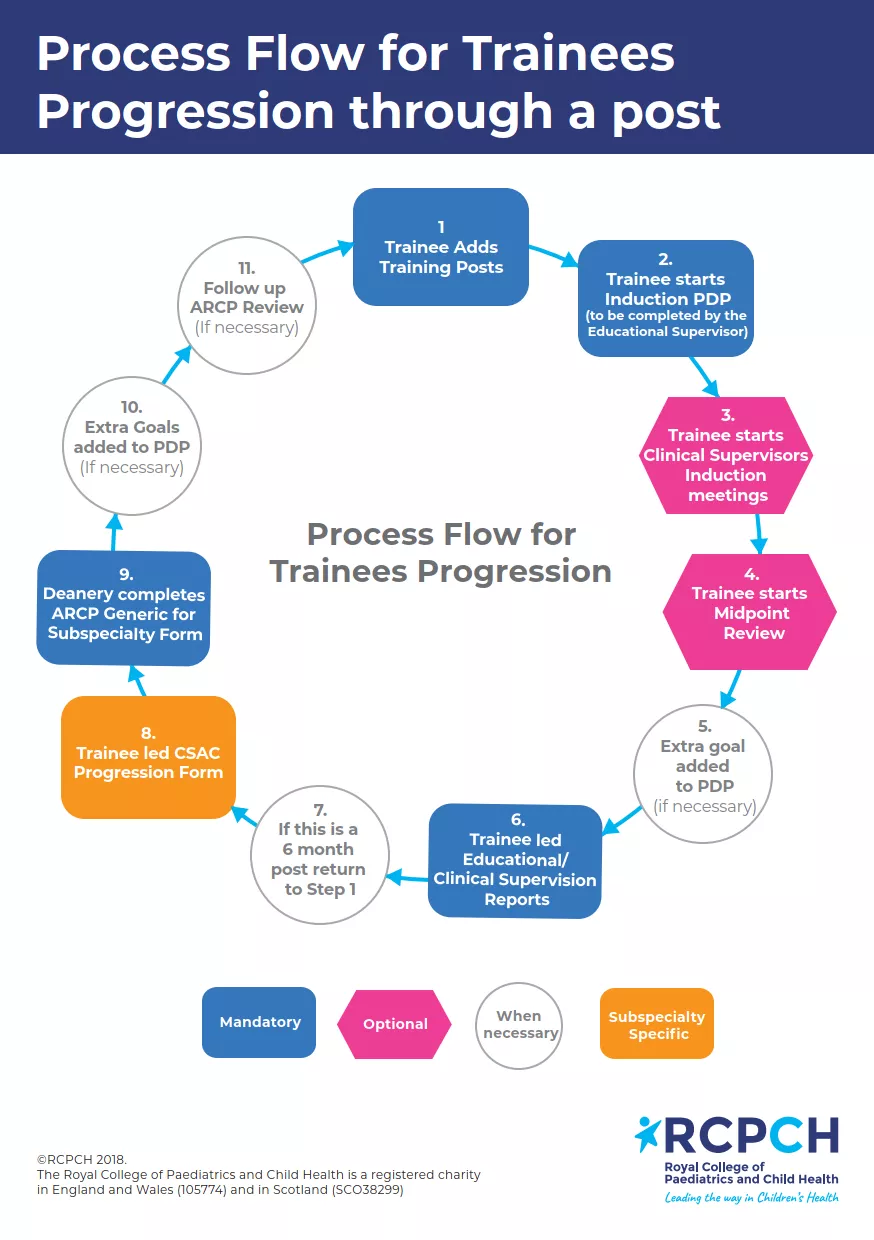
We suggest using the ePortfolio to optimise its educational benefits:
- Add your training post.
- Complete an Induction PDP. This form is started by you as the trainee and sent to your educational supervisor to complete. Upon receiving the initial part of the Induction PDP, we recommend you meet with your supervisor to discuss and confirm your PDP goals. The PDP should remain open for your training post-period.
- A clinical supervisor's induction meeting can take place after you have met with your educational supervisor. The clinical supervisor induction form is a simpler form outlining any aspects of clinical training you might want to address during the training period.
- Your midpoint review is carried out with your educational supervisor, usually in person, to review PDP goals set for the training period.
- You can add an extra goal to your PDP.
- For ARCP, an educational supervisor report must be completed and good practice suggests a clinical supervisor report too (in some areas you only need one of each every training year - check local policies)
- Six month posts end here and start again at point 1. For longer posts, carry on where applicable.
- Only for those doing official subspecialty training - SPIN and lower level training doesn't apply.
- ARCP occurs according to your deanery's local policies - check locally.
- Good practice for ARCP outcomes other than 1 is to have targets on what would help make an ARCP outcome 1 next time - these can be set up as goals in your next attachment.
- Only applicable exceptionally (most commonly for an ARCP outcome 5).
ePortfolio guidance for doctors
Progressing through training and ARCP
- The Annual Review of Competence Progress, or ARCP, is the formal review of your progress in training. It is conducted by your deanery and determines whether you are meeting your training requirements.
- The ARCP panel usually comprises programme directors, heads of school, educational supervisors and other relevant members of the educational faculty. A lay representative may also be present.
- An 'external advisor' from outside your deanery or LETB will need to review a sample of ARCP outcomes to ensure objective consistency.
Progressing through training - 'must haves'
- To progress satisfactorily in training you will need ARCP outcomes for each training grade, usually ST1-ST7. This culminates in an ARCP outcome 6 for completing training, usually at ST7.
- You will need to have covered the necessary life support requirements, (for example, completion of Advanced Life Support or Newborn Life Support courses) and maintain these. Safeguarding certification will also be required to be valid throughout training.
Sub-specialty training
A sub-specialty in paediatrics is a focused area of particular expertise in training. The generic elements of all paediatricians remain the same throughout their training, for example communication skills, patient management and patient safety. These are judged at the same standard in order to complete training.
Paediatrics offers 17 sub-specialties to link with paediatric training. You apply for sub-specialty training through competitive selection; this used to be called GRID formerly.
When you have completed sub-specialty training satisfactorily, an entry will be added on your Specialist Register with the General Medical Council (GMC) (see 'Certification' below).
How to apply for a sub-specialty.
Special interests (SPIN) modules
You are entitled to sign up to a special interest where eligible. SPIN modules are focused areas of additional training and experience that enable a paediatrician to act as a local lead in that particular area of paediatrics. SPIN modules do not carry additional certification on the doctor's entry on the GMC register.
Certification
Paediatricians are legally required to be listed on the Specialist Register at the GMC (General Medical Council) when they take up a substantive, honorary or fixed-term consultant appointment in the NHS.
There are several routes to the Specialist Register, each requiring us (RCPCH) to check you are appropriately qualified. When you apply for a specific route on to the Specialist Register, the College assesses your training, qualifications and experience and makes a recommendation to the GMC on your behalf.
CCT (Certificate of Completion of Training) - To receive a CCT and enter the specialist register you need to complete a UK training programme that carries GMC approval. You do not need to have sequential or contiguous years of training, though you must have at least one ARCP outcome plus a satisfactory ARCP outcome 6 for each specialty to get CCT recognition.
Portfolio Pathway (previously Certificate of Eligibility for Specialist Registration) - This route is open for applications where at least six months' training or a specialist medical qualification is held. This makes an applicant eligible to apply. All the skills and capabilities in the RCPCH Progress+ curriculum must be demonstrated for Portfolio Pathway in Paediatrics.
Completing training in a UK training programme - If you are completing the paediatrics curriculum in a UK training programme you will be eligible for a CCT if you have completed a UK approved training programme and are awarded an ARCP outcome 6. You will need an ARCP 'Outcome 6' for your training from your training programme. If you are in sub-specialty training, you will also need a separate ARCP 'Outcome 6' for the sub-specialty - and this will need to have been signed off by the College Specialty Advisory Committee (CSAC) in that sub-specialty. This is done via the CSAC progression form on your ePortfolio.
Certification including CCT and Portfolio Pathway
Possibilities in training
Progress+ curriculum pathway
Paediatric training following the Progress+ curriculum is over seven grades over two levels and indicatively seven years of training. it is capability-based. There are many strands to completing training and few trainees complete sequentially from ST1 to completion of training.
This flowchart helps you determine which pathway you'll follow (you can also download it at the bottom of this page).
Progress+ curricula, syllabi and resources
Less than full time
We are supportive of paediatricians working at less than full time (LTFT). Our specialty has among the highest number of LTFT doctors.
Requests to complete training levels early
To complete any level earlier than the indicative training time, the assessments numbers as outlined in the table of assessments must be met. Trainees must also agree early exit from levels with educational supervisors, programme directors, heads of school and, where sub-specialty training is undertaken, CSAC representatives..
Requests to complete specialty training early must be made at least six months in advance, ideally 12 months.
To exit core level training, trainees must hold the MRCPCH (membership exam). To complete specialty level and complete training early, trainees must have completed their START assessment and demonstrated meeting any development requirements.
Final decisions on trainees exiting a level early are dependent on satisfactory supervision reports and will be made by the Head of School at an ARCP panel. Once the decision to complete training earlier has been confirmed, a trainee will be unable to go back into training, and there is no obligation for the programme to offer a period of grace.
Acting up as a consultant
Time spent in an 'acting up as a consultant' position may be recognised as part of the training programme leading to certification (CCT).
Trainees wishing to act up as a consultant must:
- be in the final year of training towards CCT
- be 'acting up as a consultant' in the same deanery or LETB
- occupy the acting up post for at least three months (pro rata for LTFT trainees) - usually for a maximum of 6 months which can be extended at the Head of School's discretion
- have the post prospectively approved by their educational supervisor, head of school and CSAC representative
- retain their national training number
- give three months notice to their current employer (unless otherwise agreed)
- have a named supervisor for the period of the acting up post and the appropriate levels of support expected for a final year trainee
- obtain a supervisor's report covering the acting up post
- have a satisfactory ARCP outcome from their previous ARCP
- apply through ePortfolio and submit to the Head of School. Sub-specialty trainees must confirm that either they have contacted their CSAC or their TPD has done so.
The acting up post must be in approved UK training post or vacant substantive post. It is not required or appropriate that a trainee applies for out of programme approval for an acting up post.
It is not necessary to have completed your START assessment before acting up as a consultant.
Out of programme
All time out of your training must be approved by your postgraduate dean. This time can be used for research, clinical experience or a career break. Applications for out of programme (OOP) approval are governed by the Gold Guide rules and local requirements from your head of school or postgraduate dean.
Please refer to the GMC guidance, When do I need approval?.
The GMC is responsible for Out of Programme Approved Training (OOPT) and Out of Programme for Research (OOPR) only. If credit towards training is sought, it must be prospective (before the period starts). If the out of programme post is in a location that the GMC has approved for training and in the same specialty that you are working towards for a CCT, then GMC and RCPCH approval is not needed - it is the responsibility of the Postgraduate Deanery Office to check this. If the post is not GMC approved, for example outside UK, you will need RCPCH input from the RCPCH Training and Quality Board for OOPT or Academic Regional Representative for OOPR. The application needs to be submitted to training.services@rcpch.ac.uk
All OOP applications requiring RCPCH input must also include the postgraduate deanery information too and accompany the RCPCH OOP application form.
You can download the OOP application/approval letter.
The time to count confirmation in the RCPCH approval form is there is help you as a postgraduate doctor in training understand the amount of time from the post that indicatively will be suitable to support you to gain and evidence capabilities in the post. Each OOP post will be different, so we will review the OOP application such as location, your clinical placement plan during the OOP etc and will confirm from that information what time during your placement will support gaining evidence of your capabilities.
The evidence of capabilities gained during the OOP post will be reviewed at your next ARCP and this will ultimately confirm the capabilities achieved. The GMC, in any OOP sign-off say that confirmation is 'subject to satisfactory performance, which must be documented through the ARCP process.'
The GMC take this approach to help you understand how much of the post will likely support gaining experience of capabilities CCT and understand any impact it might have on future training.
As an example, a postgraduate doctor in training might be going on an OOPR for three years to complete a PhD. In the GMC confirmation, it will say three months will count towards CCT. This will help you to understand that you will gain capabilities to support your CCT which indicatively would take three months to achieve and the rest of the time is unlikely to support in evidence of capabilities towards your CCT.
In another example, a postgraduate doctor in training asking for 12 months to count towards training (eg a one year OOPT post) we would check the information available, and if happy that the whole placement would help support in gaining experience in capabilities, state in the RCPCH approval form, 12 months. This would not be a definite confirmation that 12 months would support, as ultimately you will need to evidence this and it will be up to you to collate this evidence and present at your ARCP.
Parental leave and other absences
There are statutory allowances for leave which are governed by local regulations. Any parental leave or other absence should be recorded in your ePortfolio.
Inter deanery transfers
The National Inter Deanery Transfer (IDT) process supports medical trainees who have had an unforeseen and significant change in circumstances since they started their current training programme.
The process is managed by the National IDT team (Health Education South London) on behalf of the Conference of Postgraduate Medical Deans (COPMeD), Health Education England (HEE) and all UK regions.
If you are planning to apply for an IDT process, visit https://medical.hee.nhs.uk/medical-training-recruitment/medical-specialty-training/inter-deanery-transfers-idt.
Academic training and research guidance
We are supportive of paediatricians wishing to pursue an academic career. We have established a network of Academic Regional Representatives throughout the UK to provide guidance and support to academic trainees and those wishing to undertake research alongside their clinical training.
Trainees undertaking research will generally obtain a Certificate of Completion of Training (CCT) via the conventional route, their registered specialty being paediatrics. This will usually be through the Integrated Academic Training (IAT) pathway. Recruitment for training is concurrent with the recruitment process for all trainees.
- Trainees undertaking research will generally obtain a CCT via the conventional route, their registered specialty being paediatrics. This will usually be through the Integrated Academic Training (IAT) pathway. Recruitment for training is concurrent with the recruitment process for all trainees.
- However, a small minority may seek to have their names entered on the Specialist Register via the academic route.
- The Academic Paediatrics Association (Great Britain and Ireland) welcomes members from among all those interested in academic paediatrics and those undertaking research.
- The British Academy of Childhood Disability's Strategic Research Group has developed information for trainees considering a career in academic paediatrics. The information will be of most interest to neurodisability and community trainees, but also to neurology trainees. There is information on general academic training, including its consultancy service, and a semi-automated system for locating up to date information on grant calls and fellowships relevant to paediatric disability research.
Balance between general (acute) and sub-specialty training in specialty level paediatrics training
This guidance is intended for all specialty level trainees.
- All paediatric trainees achieving CCT in the UK receive accreditation in paediatrics, and so must be competent in delivering acute paediatric and neonatal care. While trainees in many sub-specialties may not anticipate performing general paediatric on-call duties once qualified as a consultant, it is important that they recognise the value of these competencies in ensuring they can deliver safe care to the children for whom they are responsible.
- In a number of cases, a paediatrician post-CCT with sub-specialty accreditation will be employed in a service where they are expected to be competent to work on the general acute paediatric rota or undertake some general paediatric clinics/ward rounds. It is therefore essential that trainees consider this when discussing training opportunities with their supervisor.
- Out of hours working may offer training opportunities which may be more difficult to obtain within normal working hours. Examples include the acutely presenting injured child with safeguarding concerns, the sudden respiratory deterioration of an oncology patient and acute neurological presentations. The separation between “Training” and “Service” activities is artificial, and out of hours “service” time offers training opportunities to all paediatric trainees.
- The 70% guidance for time spent in sub-specialty training should be considered the minimum expectation. Although it is possible for trainees in some sub-specialties to gain sufficient experience working a lower proportion of time than this, with well-constructed training posts and good trainers, this is unusual. In this circumstance it would need much more rigorous monitoring and a requirement to demonstrate that trainees are gaining necessary experience.
- When posts are offered for sub-specialty training the CSAC should consider the proportion of time trainees will spend working within the sub-specialty prior to approval of the post. If <70% of time will be available in the sub-specialty the CSAC should have ascertained how local trainers will ensure that trainees gain sufficient experience and that appropriate mechanisms are in place to ensure this.
- The calculation should be based on 20 working weeks during a six month placement, i.e. excluding annual and study leave. The 70% recommendation is of the total hours worked. A trainee will work an average of 48hrs/week (this will be a combination of day and out of hours and the ratio will vary considerably from week to week) of which an average of 70% should be in their sub-specialty. For example a trainee may work 9-5 Monday – Friday one week (40hrs) and have no out of hours that week, thus 100% of their working time will be in their sub-specialty. A different week on the rota may expect them to work Mon-Wed 9-5 in their subspecialty (24hrs) and two x 12 hour shifts in acute paediatrics at the weekend, ie 50% of their working time in their sub-specialty.
- Sub-specialty trainees and their trainers must be mindful of the need to maintain and develop acute paediatric competencies throughout Specialty level training. It is appropriate for such competencies to be monitored by the Educational Supervisor, e.g. through WBA, and form part of the Annual Trainers Report.
- Those trainees not undertaking sub-specialty training will be expected to acquire the full range of general paediatric skills including acute care, ward round and clinic skills. The expectation is that they will achieve this through an equitable split of daytime and out of hours when working alongside subspecialty trainees. If a post is normally part of an out of hours rota then trainees in that post are expected to contribute to that rota.
- For doctors training less than full time, the expectation is the same as above pro rata and includes the full range of out of hours duties (night time, evening and weekend pro rata).
- While this mainly sets the expectations for sub-specialty trainees, it is also the expectation that specialty level trainees in general paediatrics, sharing rotas with sub-specialty trainees, should not be disadvantaged. Their access to daytime training including outpatients is equally important. In the event of rota gaps, Trusts should deal with this robustly and find alternative methods of acute cover so as not to compromise the training of both sub-specialty and general paediatric trainees.
Rationale
It is essential that we ensure that both specific acute capabilities are achieved and also the generic skills in the management of acutely ill and unscheduled patients when direct supervision is less available. In some units there may be a ‘quid pro quo’ arrangement. For example, the sub-specialty trainee does a certain amount of time covering the general acute service during the week in exchange for the general paediatric team covering for the sub-specialty emergency admissions at times when the sub-specialty trainee is unavailable, for example in out-patients.
Previous guidance from the College Specialty Advisory Committees (CSACs) stated that sub-specialty trainees should spend 70% of time working within their sub-specialty. A National Survey of Paediatric Trainees undertaken by the RCPCH Trainee Committee in 2011 identified that approximately 30% of trainees in sub-specialty training reported spending 70% of their working time within their sub-specialty. These trainees were more likely to report perceived difficulties in obtaining sub-specialty capabilities compared to trainees working less than 70% of their time within the sub-specialty.
Previously the College has recommended that no more than 33% of hours worked by all trainees should be in the delivery of emergency out of hours care, equating to ~16 hours of the 48 hours maximum working time and ~ equating with the advice provided by the CSACs. The time requirement of no more than 16 hours out of hours may be less relevant to 24 hour sub-specialties, eg PICM and ED.
Safe cover capabilities
All of the following capabilities are essential for safe cover.
The RCPCH does not believe that ST1 and ST2 trainees should work on the middle grade rota. If there is no-one on-site with the defined capabilities for safe cover, we would expect a doctor at the consultant or equivalent grade to remain resident to provide the safe cover.
While this guidance is intended for trainees who are working at ST3, it is equally applicable for more senior trainees returning to work after a gap, for example, parental leave or research without acute commitment.
The below lists each assessment standard theme and its safe cover competencies for Core training.
- Advocate
-
- Understand the duties and responsibilities of a paediatrician in the safeguarding of babies, children and young people; and supporting parents and carers
- Understand the limitations of their competence at this stage of their training and know where and when to ask for help, support or supervision - particularly in relation to safe recognition and management of seriously ill children and young people
- Understand and follow the principle that all decisions are to be made in the best interests of the child or young person in their care
- Understand the concept of advocacy for a healthy lifestyle in children and young people and for the protection of their rights
- Understand the responsibility of paediatricians to consider all aspects of a child's well-being, including biological, psychological and social factors
- Knowledge
-
- Know about the initial assessment and management of common causes of admission to hospital due to psychological distress such as self harm, somatic symptoms of distress
- Know about the effects of substance abuse
- Recognise the mental health components of paediatric illness
- Know the aetiology, pathophysiology, presentation and management of common and serious childhood conditions
- Know the patterns of normal development from birth to adulthood
- Be able to recognise and treat accidental ingestion and deliberate self-poisoning
- Clinical skills
-
- Be able to examine children and young people accurately and sensitively in appropriate settings
- Recognise case histories which suggest serious or unusual pathology in children
- Recognise the diseases and host characteristics which make certain presentations life-threatening in children and know when to ask for help
- Recognise presentations of common disorders in children and initiate management
- Be able to formulate a differential diagnosis and appropriate management plan
- Assessment of the newborn at birth including recognition and initiation of treatment of sepsis, respiratory distress, cardiac conditions, surgical problems, dehydration, hypoxic ischaemic encephalopathy
- Recognise, assess and initiate management of acutely ill or collapsed child in particular shock (including septic shock), anaphylaxis, unconscious patient, acute asthma, acute continuing seizures, meningitis, encephalitis, acute abdomen
- Technical skills
- Prescribing
-
- Be able to prescribe safely and legibly for the newborn and for children of all ages
- Know the approved indications and justification for prescribing drugs in common paediatric problems
- Be able to calculate drugs accurately according to specific dose for weight or age/weight range or on a specific dose/specific area basis for drugs and fluids
- Know how to find out information necessary for safe prescribing through the use of paediatric formularies and pharmacy liaison
- Know how to use the local and national guidelines for the relief of pain in children
- Understand the rationale for prescribing common antimicrobials
- Be able to apply the national and local guidelines on prescribing paediatric intravenous fluid
- Safeguarding
-
- Be able to recognise and outline the management of children in need of protection
- Recognise features in presentation, where child protection may be in an issue for example where there are patterns of injury, delay in presentation, inconsistencies in the history
- Recognise where families are distressed and need help to prevent child abuse
- Be familiar with the different categories of abuse and recognise that they may occur together: physical, emotional, sexual, neglect, fabrication or falsification/induction of illness in a child
- Know the local guidelines and follow the procedures
- Keep accurate records of all findings and communications with the child, family members and all other professionals
- Be able to record clearly the results of an examination of a baby, child or adolescent using body charts
- Recognise the importance of noting all observations of the child's demeanour and interactions with parents and carers
- Understand the need to initiate a safe response where abuse is suspected, while treating the family with respect and courtesy at all times
- Have attended child protection awareness training in accordance with Trust policy
- Management and leadership
-
- In complex difficult communication situations with children and families show awareness and have began to develop strategies to respond particularly in complex family situations
- Be able to prioritise tasks in personal and professional contexts for example in medical emergencies
- Ensure effective hand-over procedures and clear communications with colleagues to ensure the continuing good medical care of patients
- Lead the team in initiating resuscitation
- Teaching, supervision and mentoring
-
- Show a commitment to their continuing professional development and respond positively to requests for enquiries or critical incident reports and to outcomes of reviews, assessments and appraisals of their performance
- Multidisciplinary learning
-
- Understand the need to engage effectively with professionals in other disciplines and other agencies
- Understand the need for open and non-discriminatory professional working relationships with colleagues
- Recognise the needs for timely senior support in serious clinical situations and be effective in requesting this
- Professional attributes
-
- Know where to find assistance in the case where a child or family member may not speak English
- Have strong communication and interpersonal skills to enable them to work effectively with patients and their families, and colleagues in multi-professional and multi-discipline teams
- Be able to discuss the indications, benefits and adverse events of a procedure to patients, relatives and carers that will allow informed consent for procedure which the doctor is competent themselves to perform
- Demonstrate compassion, empathy and respect for children, young people and their families
- Law and ethics
-
- Know the local and national guidelines for obtaining informed consent
- Begin to develop effective written communications with patients and their families, with colleagues and with other professional organisations
- Professional development
-
- Demonstrate a commitment to the highest standards of care and ethical and professional behaviour within their speciality and with the medical profession as a whole
Your Trainee Committee
This is your best way of interacting with the RCPCH with a collective voice. The Trainee Committee and its Executive give you an opportunity to raise training issues with the College. There are representatives for subject areas and across the UK.