This page has guidance for candidates preparing for the exam. Since October 2020, the exam has been delivered remotely via an online platform.
- Aim
- How remote delivery works
- Understanding the adapted exam
- Helping you with your revision
- Format
- Exam circuit
- Timing
- Marking scheme and the pass mark
- Candidates known to examiners
- Stations one and two: Communication skills stations
- Station three: Data interpretation
- Station four: Short Clinical
- Station five and six: Focused history taking and management planning
- Station seven: Child development assessment
- Station eight: Safe prescribing
- General instructions for candidates
- Downloads
Aim
To assess whether candidates have reached the standard in clinical skills expected of a newly appointed General Practitioner who has completed a short period of training in paediatrics, and who displays a special interest in paediatrics. Scenarios are generally written with reference to the candidate being a GP.
Candidates are expected to demonstrate proficiency in:
- communication
- history-taking and management planning of chronic conditions
- establishing rapport with both parents and children
- physical examination (conveyed to examiners verbally following a structured approach)
- child development
- clinical judgement
- organisation of thoughts and actions
- knowledge and understanding of common problems in child health
- professional behaviour
- ethical practice
- interpretation of data
- safe prescribing.
How remote delivery works
As of October 2020, the DCH Clinical is delivered remotely. We now use an online system called OSLER.
You can find out more in these guides:
- DCH Clinical remote delivery - anchor statement 2020 - download below
- DCH Clinical remote delivery - candidate information 2023 - download can be found at bottom of page.
- Requirements for remote delivery (on our DCH Clinical - How to apply page) - this covers what you wil need, including internet connection, web browser and device/computer
Our video, created in November 2022, explains how remote delivery via OSLER works. (You can see our video explainer on how the adapated exam works in the section below.)
Understanding the adapted exam
Historically, DCH Clinical was delivered in person and involved real patients in some stations. Since October 2020, we are delivering the exam online, and clearly it is not possible to undertake a fully authentic physical examination or developmental assessment of a child through an online system.
The DCH Board and Clinical Assessments team have developed scenarios aimed at assessing these skills in different ways. As a candidate, you are now expected to verbalise your approach to a physical examination or assessment of a patient. This approach presents new challenges, and will require practice with a colleague so you can demonstrate to examiners that your approach to a patient is accurate and well structured and that it takes into consideration the patient's needs.
Video explainer on the adapted exam
This video, recorded in October 2020, explains how the adapted exam works. (You can see our video explainer on the online platform, OSLER, in the section above.)
Helping you with your revision
The RCPCH has a range of support and resources for candidates including exam preparation courses and textbooks that may be of interest whilst you are revising.
Format
The DCH Clinical includes:
- 16 objective assessments of each candidate across eight stations (Part A and Part B)
- structured testing of communication skills
- observed history taking and discussion of management
- one clinical examination station (candidates required to verbalise approach)
- testing of skills in developmental assessment and neurodisability assessment
- interpretation of data
- safe prescribing.
Exam circuit
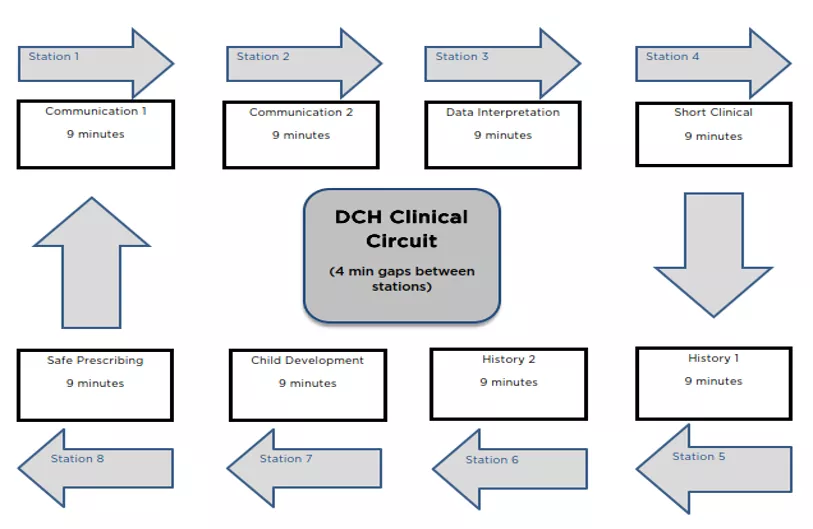
This diagram shows the eight stations and timings of the exam circuit.
On AM exam day, you will typically need to be logged into Osler system at approx 09:00 UK time. The AM circuit begins at approx 10:00.
There are eight stations:
- Communication (x2)
- Data interpretation
- Short clinical station
- History (x2)
- Development station
- Safe prescribing station
Each station is nine minutes long. There is a four-minute break between each station. The total time should not be longer than two hours but may be longer if there are any delays.
Each station is marked across Part A and Part B.
There is one examiner for each station. There's an additional senior examier who provides quality assurance and back up.
When you have completed your exam circuit, you will automatically join a debriefing meeting with the Senior Examiner and a member of the Clinical Assessments team.
Timing
All candidates can expect to be examined for the full allotted time. Strict time keeping is essential. The invigilators will indicate the system of time signalling. You will be notified when you can begin reading the materials required to prepare for each station and when to start your stations. If there are delays within the circuit candidates will be required to wait for further instructions from the support team.
More details on each station:
Communication
- Candidate reads instructions during reading time (4 minutes)
- Candidate starts station and has nine minutes with role player and examiner
- At six minutes candidate receives a warning that three minutes are remaining
- At nine minutes station ends
Data interpretation
- Candidate reads instructions during reading time (4 minutes)
- Candidate starts station and has nine minutes with examiner
- At six minutes candidate receives a warning that three minutes are remaining
- At nine minutes station ends
Short clinical
- Candidate reads instructions during reading time (4 minutes)
- Candidate starts station and has nine minutes with examiner
- At six minutes candidate receives a warning that three minutes are remaining
- At nine minutes station ends
History
- Candidate reads instructions during reading time (4 minutes)
- Candidate starts station and has six minutes with role player to take a history
- At six minutes candidate receives a warning and the history taking with the role-player ends and communication with the examiner begins (summary of history and management plan provided)
- At nine minutes station ends
Development
- Candidate reads instructions during reading time (4 minutes)
- Candidate starts station and has nine minutes with examiner
- At six minutes candidate receives a warning that three minutes are remaining
- At nine minutes station ends
Safe prescribing
- Candidate reads instructions during reading time (4 minutes)
- Candidate is permitted to read the scenario and begin to refer to the BNFC during reading time (approx additional 3 minutes of reading once station has started)
- Candidate starts station and has nine minutes with examiner
- Candidate must have completed process of highlighting errors in the prescription and correcting them before end of first six minutes
- At six minutes candidate receives a warning that three minutes are remaining and must have summarised the prescription corrections and have begun to discuss further aspects relating to knowledge skills and attitudes to prescribing
- At nine minutes station ends
Marking scheme and the pass mark
At the end of each station the examiner will make an overall judgement as to whether or not the candidate’s performance was as below.
| Category | Mark | Comment |
|---|---|---|
| Clear pass | 12 | Demonstrates the competencies being tested in the station; this includes candidates who have satisfied the requirements and those who excel |
| Pass | 10 | Elements of the performance that are not as good as expected but that are not sufficient to give a fail grade; where a candidates exhibits some minor failings |
| Bare fail | 8 | Has made an inappropriate number of minor errors or some more important errors |
| Clear fail | 4 | Poor performance in one or several areas |
| Unacceptable | 0 | For unprofessional or dangerous behaviour (rough handling of a child, rudeness, etc.) or for extremely poor performance |
Anchor statements outlining the expected general standard for each station are provided to all examiners in order to aid them reach their overall judgements.
There will be a total of 16 judgements. Candidates will fail if they do not obtain a total of 160 marks.
The final pass/fail mark can be raised at the Senior Examiner Board Meeting held after each exam period.
If a candidate’s behaviour is unprofessional, under these exceptional circumstances, candidates may be stopped by the Senior Examiner from continuing with the examination.
Candidates will not fail on the basis of a single encounter (unless there is unprofessional behaviour of sufficient severity), but will be marked on an accumulation of marks.
Candidates known to examiners
If an examiner feels that this creates a significant difficulty with a particular candidate they will highlight this with the Clinical Assessments team. In this event the Senior Examiner may step in to examine on that station.
Stations one and two: Communication skills stations
Time of station
Two stations of nine minutes
Aim
To test the ability to communicate appropriate and factually correct information in an effective way within the emotional context of the clinical setting.
Communication is most frequently with a surrogate parent or health care professional or adolescent. A candidate may be asked to talk to a real parent and/or child, a health professional, or a member of the public.
The task
There are six main patterns of communication scenario:
- information giving (eg please tell this parent about the diagnosis)
- consent (eg please explain why you need to do a lumbar puncture with a view to obtaining consent)
- critical incident (eg please talk to the parent of the child who has been given the wrong drug)
- ethics (eg please discuss the problem as Anna has refused to have any blood tests)
- education (eg please explain to the health care professional so that she can deal with the situation)
- candidates may be asked to explain use of common medical devices; a manikin or model may be used in the station.
Candidate information
Written information will be provided about your role, clinical background and the task required. This is provided to read through the assessment platform.
You will not be required to examine any patient; information including growth charts and results of investigations may be provided if relevant.
Assessment
Candidates will be marked on their communication skills.
This means that a candidate needs to:
- select the most appropriate information to communicate
- provide information that is correct
- explain issues in an appropriate way without jargon
- respond and adapt to the emotional context of the station.
It is not a test on the amount of information conveyed in nine minutes. In some scenarios, the task would normally take more than nine minutes and may not be completed. Candidates should be penalised for asking irrelevant questions or providing superfluous information.
Candidate tips
- Ensure you read the scenario carefully.
- Establish what the 'parent'/health professional already knows in order to give you a baseline from where to start.
- Establish what the parents concerns/anxieties/question are
You are not expected to examine in this station.
Sample communication skills scenario
Sample instructions to candidate
This station assesses your ability to give information to a parent/patient.
You are: A GP working in a small rural market town
You will be talking to: Jane Smith the teenage single mother of Jason, aged 18 months.
Task: To explore her concerns about febrile convulsions
Setting: GP Surgery
Other information: You are not expected to gather the rest of the medical history during the consultation.
The examiner will have both the candidate sheet and role player sheet.
Examiner marking criteria: Candidate should be able to:
- clearly explain febrile convulsions
- explain good long-term prognosis.
- show empathy for parent concerns.
Station three: Data interpretation
Time of station
One station of nine minutes
Aim
To assess ability to interpret data in a clinical context
Task
To interpret data provided and discuss with the examiner the implications of the data and an appropriate management plan
Examples of data include blood tests, urinalysis, audiograms, growth charts, diabetic diaries, peak flow charts and laboratory reports etc.
Candidate information
Written information will be provided about the task. This is provided to read through the assessment platform.
Timing and marking of the station - this will be:
- If you have completed answering the examiner’s questions in less than nine minutes, the examiner will check that you have finished.
- If you have, you should remain in the examination room until the end of the allocated time.
Candidate tips
- Ensure you read the instructions carefully as they will inform you of what is expected.
- Do not spend too long reading the data – remember there are questions for which you need to write down the answer.
Sample data interpretation scenario
Sample instructions to candidate
Task: to interpret data in the clinical context provided.
Discuss with the examiner the relevance of the data in the diagnosis and management.
This is a nine-minute station. You will have four-minutes beforehand to read this sheet and prepare yourself.
You may take the sheet with you into the station but you must return it at the end.
Role: You are a GP
Setting: GP Surgery
Task: Interpret data
Candidate information: A 14 year old girl has a five day history of fever accompanied by tiredness, anorexia, headache and a sore throat. On examination, she has pharyngitis, generalised lymphadenopathy and palpable spleen.
Investigation:
- Hb 1.9 g/dl (11.0 -17.0 g/dl)
- WBC 19.2 x109/L (4.5 - 13)
- neutrophils 2.6 x109/L (1.5 – 6)
- lymphocyte 12.3 x109/L (1.5 – 4.5)
- monocytes 2.0 x109/L (0.15 – 1.3)
- eosinophils 2.2 x109/L (0.05 – 0.8)
- basophils 0.1 x109/L (0.02 – 0.12)
- atypical mononuclear cell 33%
- Platelets 157 x109/L (150 -450)
Station four: Short Clinical
Time of station
One station of nine minutes
Aim
To assess clinical examination skills and interpretation of clinical signs. There is only one examiner in each station (no patient is used in the online exam).
Candidates will be tested in any of the following areas:
- cardiovascular
- abdomen
- respiratory
- surgical
- neurology
- other, eg endocrine, eyes, skin, etc.
Candidate information
Each candidate will be given a scenario to read through the assessment platform. Once the stations begins the examiner will repeat the task and ask the candidate to verbalise their approach to the examination of the child as detailed in the scenario. As candidates provide correct approach to the examination of the child the examiner will provide clinical information in relation to the patients condition. The examiner may intervene at any time, and will ask the candidate questions about clinical findings and their interpretation or management implications at any stage during the nine-minute station.
Details about what is expected of candidates when performing a clinical examination of a child (Short Clinical station) and a developmental assessment of a child (aged 0-5) can be found at the bottom of this page.
Example: “This is Meg who is six months old and her parents are worried about a swelling of her umbilicus. Please examine her abdomen."
Candidate tips
- In the Short Clinical station you could be presented with a patient with health issues across different systems – CVS, RS, GI, thyroid, etc.
- It is designed purely to test your clinical examination skills.
- There is no need for you to take a history.
- There is no patient in this station
- Additional resources may be provided through the assessment platform such as video clips or images
- Listen or read instructions carefully and do what is asked. Answer any questions posed by the examiner.
Station five and six: Focused history taking and management planning
Time of station
Two station of nine minutes each
Aim
To assess the candidate’s ability to take a focused history, summarise and formulate a management plan.
The task
To review chronic disease management. This will be with a role player. The candidate will be expected to take a focused history. Candidates will not be required to examine the patient; relevant information including growth charts and results of investigations may be provided. After taking the history, the candidate will discuss a management plan with the examiner.
Candidate instructions
The aim of the station is to take a history focussed on the child’s chronic condition. If the role player ask questions during the consultation, it may be appropriate to answer these. However, the role-player should be discouraged from asking any questions about management of their condition/child’s condition.
Candidate information - written information will be provided about the task required. This is provided through the assessment platform.
Timing and marking
- The total time taking a history from the patient will be a maximum of six minutes. The examiner should then award a mark for this section.
- A time warning will be issued after six minutes.
- The examiner will then discuss the case with the candidate for the remaining three minutes. A mark should be awarded for this section.
If you have reached the end of the history-taking in less than six minutes, the examiner will check that you have finished. Should you finish early, the examiner will ideally wait until the six minutes have elapsed before continuing the examination. Candidates can be told to take the time to compose and reflect over their notes. The role-player will remain in the room during the entire nine minutes.
Candidate tip
- It is advisable to use the break between stations to write down areas you wish to cover, in order to structure your history taking.
- Ensure you ask about past medical history and drug history
- Ensure you leave enough time to discuss management.
Sample focused history taking and management planning scenario
Sample instructions for the candidate
The task with the parent/role-player is to take a focused history.
The examiner will focus on your understanding of chronic disease management.
This is a nine-minute station. You will have up to four minutes before the start of this station to read this sheet and prepare yourself. You may make notes on the paper provided.
When the bell sounds, you will be invited into the examination room. You may take this instruction sheet with you.
You will have six minutes to take a history from the patient, with a warning after six minutes. The examiner will observe your history taking during this time.
You will then have three minutes with the examiner for discussion.
You are not required to examine the patient.
Role: You are a GP
Setting: GP surgery
You are talking to: Gregory a six-year-old boy and his mother.
Task: Take a focussed history for this case and discuss your management plan with the examiner.
Background information: George is attending your surgery for the first time with his mother. His family have recently moved to the area. George has diabetes.
Any other information: George has two older siblings
Station seven: Child development assessment
Time of station
One station of nine minutes.
Aim
To assess the candidate’s ability to perform developmental assessment by:
- clinical developmental assessment of the child
- brief assessment of neurodisability if present
- supplementary history taking from the parent if appropriate
- any other material provided at the station, e.g. the parent held record, growth chart.
Candidate information
The emphasis is on clinical developmental assessment. Candidates are expected to make an assessment of development and recognise neurodisability. Candidates should be able to discuss the implications of their findings and the child’s management.
Suitable toys and other equipment are provided within an image that can be viewed on the assessment platform. You will need to inform the examiner of your selection of the most appropriate tools for the developmental assessment.
General points:
- There is no patient in this station. The station is scenario led. The child mentioned within the scenario will have a developmental age of less than four years.
- Candidates are not expected to perform psychometric testing.
- Within six minutes the candidate should be able to highlight to the examiner which tests they would undertake in relation to the indicated area of development and determine the nature and severity of any problem, and the degree of confidence with which this assessment is made.
- The candidate should be able to outline the main areas of management and demonstrate their knowledge of the roles of the members of the multidisciplinary team dealing with child developmental problems.
- The candidate should understand the principles of vision and hearing assessment.
Timing and marking of the station
- Candidates should aim to have completed their verbalised approach to the examination of the patient within the first six minutes. The examiner will then award a mark for this section.
- A time warning will be issued after six minutes during the examination.
- The examiner will discuss the findings and interpretation with the candidate for the remaining three minutes. A mark will then be awarded for this section.
Candidate tips
- Listen/read instructions carefully
- This is not a history station – purely examination
- You are not allowed to ask the age of the child unless specifically stated in the information provided
- It is important to be systematic
- Focused usually on one area of developmental examination
Station eight: Safe prescribing
Time of station
One station of nine minutes.
Aim
To assess ability to accurately address errors in a prescription paying particular attention to correct dosage according to a child’s age and weight and appropriate to the described clinical scenario, and to understand the implications of this prescribing
Task
To correct an inaccurate prescription and discuss with the examiner the implications of your decisions with reference to indication, dose calculation, contraindications, potential adverse reactions and specific issues related to taking the medication.
Please familiarise yourself with general guidance and prescription writing; these can usually be found in the first few pages of the BNFC and you should read them before attending the exam.
Examples could include treatment of asthma, infections, epilepsy.
Candidate information
Written information will be provided about the task required. This is provided to read through the assessment platform.
Timing and marking of the station
- The total time for the candidate to complete the process of identifying errors in the prescription will be a maximum of six minutes. The examiner will then award a mark for this section.
- Once you have finished review of your prescription, the BNFc must no longer be referred to for the remaining time. Candidates are permitted to refer to the BNFC during their reading time for the station and during the first three minutes of the station but must stop reading or referring to the BNFC in the final six minutes of the station.
- A time warning will be issued after six minutes indicating that the candidate must begin discussion on further considerations in relation to safe prescribing with the examiner.
- The examiner will discuss the implications of your decision with the candidate for the remaining three minutes. A mark will then be awarded for this section.
Candidate tips
- Check dosage – you are expected to refer to BNFC extract
- Ensure you prescribe the right drug as prescribing an inappropriate drug could lead to a fail.
- Look at Paediatric Prescribing Principles: an eLearning course for paediatricians and all health professionals with a role in prescribing drugs for children and young people.
Sample safe prescribing scenario
Sample instructions for the candidate
- To prescribe effectively and in context using the BNFc provided
- To discuss with the examiner your knowledge and understanding of the medications prescribed
This is a nine minute station. You will have up to four minutes before the start of this station to read this sheet and prepare yourself.
Role: You are a GP.
Setting: GP surgery
You have seen: Laura Smith, a fourteen year-old girl and her mother. Laura has had three episodes of generalised fits. Her EEG has confirmed that she is suffering from epilepsy. Mum is keen to commence her on medication to prevent further fits. Please identify the errors in the prescription and then prescribe a suitable antiepileptic agent for Laura. Her weight is 50Kg and height 160cm.
Task: Identify the errors in the prescription using the BNFc provided
With the examiner: Discuss issues of safe prescribing
Equipment needed: BNFC, Prescription pad/Hospital Drug chart
General instructions for candidates
- Please allow plenty of time to join the online exam. Once the circuit starts, it will be almost impossible to let you catch up if you are late – although we will always do our best to do so. We will not allow your late arrival to affect the performance of other candidates
- Please note exams can often run over time so please allow for this.
- Please ensure that you switch all electronic devices to silent / no vibrate including mobile phone before logging onto the exam. Mobile phones or tablets are permitted for use in the Safe Prescribing station only if candidates are accessing the BNFC electronically but relevant sections of BNFC are included as extracts in the station. Please remember to bring photo ID with you as this will be checked in your first station on the circuit.
- Candidates may have refreshments/water during the exam.
- Remember, we are not examining to in order to find outstanding candidates. We are looking for candidates who meet the standard required for success. The standard is clear. We require successful candidates to demonstrate that they can perform at the level expected of a new, competent GP. We do not try to trick candidates but look to see how you are likely to perform when going about your usual work.
- Candidates are expected to dress in a manner appropriate to a normal working day in clinical practice, and to familiarise themselves with the principles of infection control.
- Please read any instructions given to you at the start of the station very carefully. There will be four minutes to read this. Finish reading instructions when the invigilator announces the start of the station – you will be unlikely to be able to perform at the station without knowing the instructions.
- Examiners will meet before the start of the examination to determine the pass/fail criteria. Examiners are given guidance notes to mark. Any examiner who departs from these guidelines will have their marking reviewed and unless there is good reason altered. In addition, an extra examiner may be present to monitor examiner performance to check that the exam is fair and consistent.
- You may come across a station where videoing is in progress: this is for examiner training and for performance checking of examiners only. Any video taken is not used for candidate marking.
- You may also come across observers. These individuals may be examiners in training or may be others such as clinical tutors who need to better understand the examination in order to help their trainees. Observers are normally invisible within the assessment platform and are asked to mute themselves before joining.
- You must not communicate with other candidates on the same or other examination cycles.
- When you have finished, please remember to remain for the candidate debriefing session.
- You must not provide details about the stations to commercial organisations or post them on the Internet without permission of the College.









